HR Connect
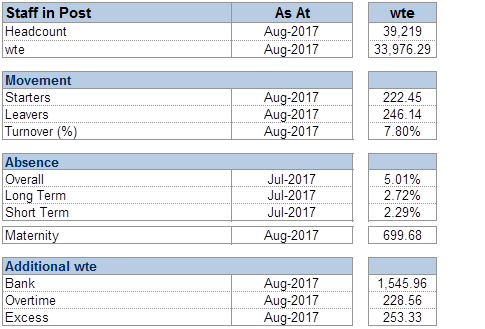
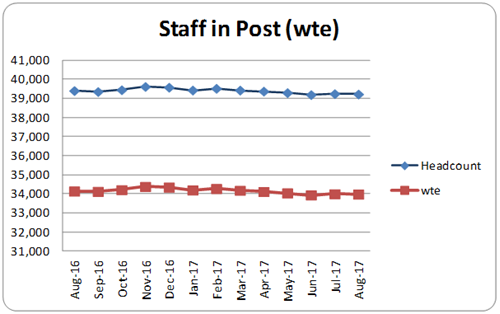
Staff in Post Trends
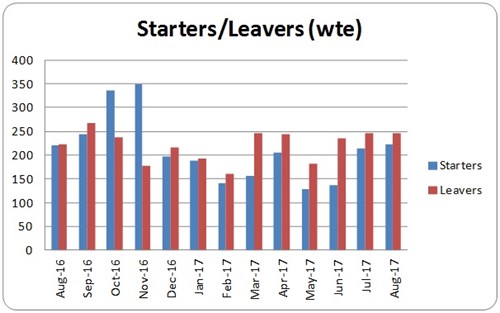
Starter and Leavers Trends
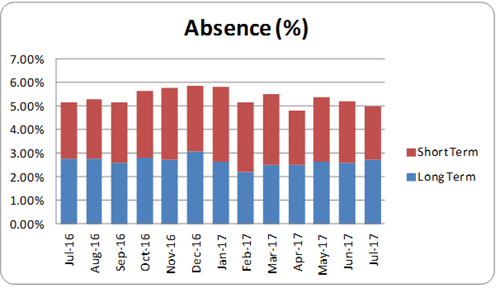
Absence % Trends
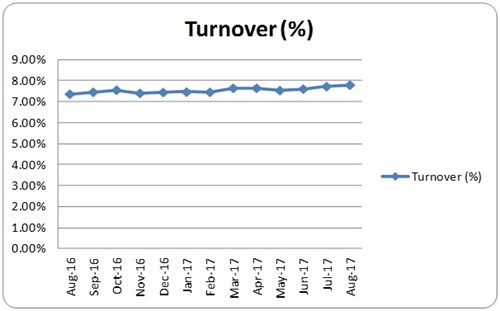
Turnover % Trends
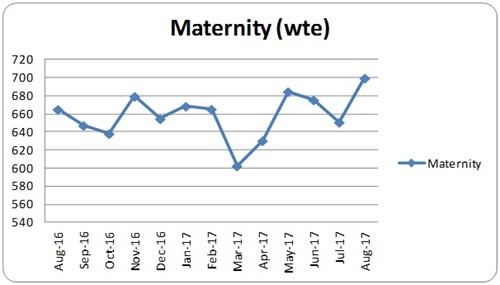
Maternity Leave
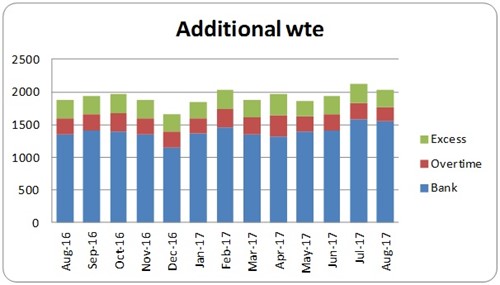
Additional Staffing
Was this helpful?
Workforce Analytics provides workforce statistics for both internal and external use. The information they supply is used throughout the organisation and is provided externally to the Scottish Government and in response to Freedom of Information requests.
Workforce Analytics also maintains and supports NHS Greater Glasgow and Clyde’s HR system, which is accessed by over 600 staff to obtain personnel, recruitment and training information across the organisation. In addition the team are involved in supporting the implementation of the new national Electronic Employee Support System (eESS).
Most of Workforce Analytics monthly reports are circulated either through MicroStrategy or SharePoint. Should you require access or wish to discuss any of our reports, please contact: workforce.information@ggc.scot.nhs.uk
The Trade Union (Facility Time Publication Requirements) Regulations 2017 require public sector employers to publish information relating to facility time taken by union representatives within their organisation. The reporting period runs from 1 April to 31 March and reports require to be published by 31 July each year.
ISD Scotland Workforce Information
NHSScotland’s Information Services Division (ISD) provides health information, health intelligence, statistical services and advice that support the NHS in progressing quality improvement in health and care and facilitates robust planning and decision making.
In order to support this work ISD collects a variety of information on staff employed in NHS Scotland. This information is used by ISD and NHS Boards to support local, regional and national workforce planning.
The latest National Statistics publication of Workforce Information can be accessed using this link and provides data at national and board level under the following headings
- All staff in post
- Vacancy numbers for nursing and midwifery, allied health professions, consultants and pharmacy staff
- Staff Turnover
- Nursery and midwifery student intakes, students in training and progression rates
- Clinical nurse specialists
- Consultant contract
- Dental workforce
More Information
Was this helpful?
Contact Us
- Tracey Carrey, Interim Workforce Planning & Analytics Manager
Telephone 0141 278 2682 or email: Tracey.Carrey@ggc.scot.nhs.uk
Workforce Analytics Team
- Ian MacRae, Workforce Analytics Lead
Telephone 0141 278 2680 or email: ian.macrae@ggc.scot.nhs.uk - Lisa Thomson, Workforce Planning Lead
Email lisa.thomson16@ggc.scot.nhs.uk - Marion Byrne, Workforce Information Analyst
Telephone 0141 278 2681 or email: marion.byrne@ggc.scot.nhs.uk - Tom McMeekin, Systems Analyst Programmer
Telephone 0141 278 2684 or email: thomas.mcmeekin@ggc.scot.nhs.uk - Lauren McGuire, Medical Staffing Workforce Information & Planning Advisor
Email: lauren.mcguire2@ggc.scot.nhs.uk - Shebina Bhatti, Workforce Analyst
Telephone 07813402694 or email: shebina.bhatti@ggc.scot.nhs.uk
eESS Technical Team
- Evelyn Gourlay, Workforce Data Quality & eESS Lead
Telephone 01475 504799 or email: evelyn.gourlay@ggc.scot.nhs.uk - Wilma McAulay, Workforce Data Assistant
Telephone 01475 504303 or email: wilma.mcaulay@ggc.scot.nhs.uk - Sandra Macer, Workforce Data Assistant
Telephone 01475 504688 or email: sandra.macer@ggc.scot.nhs.uk - Carole McFarlane, eESS Data Assistant
Email: carole.mcfarlane2@ggc.scot.nhs.uk
eESS Support Team
- Nicola McDonald, Data Assistant
Email: nicola.mcdonald@ggc.scot.nhs.uk - Jacqueline Graham, Operational Lead
Telephone 07870917741or email: jacqueline.graham@ggc.scot.nhs.uk - Claire Louise Gilles, eESS Data Assistant
Telephone 0141 278 2700 or email: clairelouise.gillies@ggc.scot.nhs.uk - Eilidh McHugh, eESS Data Assistant
Email: eilidh.mchugh@ggc.scot.nhs.uk - Dean Brandon, eESS Data Assistant
Email: dean.brandon@ggc.scot.nhs.uk - Kirsty McNeil, Bank Administrative Assistant
Email: kirsty.mcneil2@ggc.scot.nhs.uk
Workforce Forms Guidelines
There is a range of guidance available to help managers provide the workforce information that is required for good staff governance.
The information provided will be recorded into HR, Payroll and finance systems in line with Data protection guidelines.
Please note the following link is available internally only via Staffnet.
More Information
Was this helpful?
Strategic Influencing
Influence is Critical
Being able to influence effectively at all levels across the organisation in a way that builds relationships for today and for tomorrow is a critical leadership skill.
Being able to influence effectively supports NHS Greater Glasgow and Clyde to fulfill our purpose, develop our culture and capability and to work efficiently with other agencies.
We have developed learning videos to offer some simple tools and approaches to develop your influencing skills.
- Behavioural Styles
- Mapping Best Practice
- Principles of Power
- Stakeholder Influencing Process
- Stakeholder Mapping Process.
To view these videos, please visit our Staffnet pages.
Further development in the form of a one day Strategic Influencing Skills workshop and access to one-to-one Influencing Coaching sessions may be available – please discuss with the OD Team and your line manager.
Online Leadership Sessions
Short, focused sessions can be a useful way of learning about new ways of thinking or good practice from others without undertaking a longer development programme.
Our online leadership sessions focus on specific leadership topics or skills and are designed to offer a “taster” or introduction rather than deep knowledge or learning.
Online leadership sessions are aimed at mid/senior level or those who have completed a longitudinal leadership programme. Places are allocated on a first come first served basis.
2026 Calendar
- Wednesday 25th February 08.30am – Civility Saves Lives – Making Life Work Better, Dr Michael Murray
- Tuesday 3rd March 08.30am – Facilitating Productive Meetings, Maria Moreno, M Potential
- Thursday 23rd April 08.30am – Co-Created Relationships and the Drama Triangle, Dr Sandra Wilson, Insightful Journey
- Tuesday 26th May 08.30am – Having Impact and Influence, Laurence Clarke, Taylor Clarke
- Thursday 25th June – 3.30pm – How To Stop Burnout, Andrew Pain
- Wednesday 26th August – Compassionate Leadership, Moon Li, Kapow Coaching
- Wednesday 23rd September 08.30am – The Power of Curiosity Using A Coaching Approach, Maria Moreno, M Potential
- Thursday 29th October – Civility Saves Lives Making Life Work Better, Dr Michael Murray
- Thursday 26th November – 3.30pm – Imposter Syndrome, Andrew Pain
- Tuesday 15th December –
Everything offered by OD aims to be inclusive for all staff. Please email Lisa Donnelly or the OD Team, if we can help with any arrangements, for instance for staff with a sensory impairment, that would make our programmes or materials easier for you to access.
Coaching
Coaching is a person centred, future focussed and positive development approach.
It is increasingly used in all business settings, including the Health Service across Scotland. It has been shown to be a cost-effective and holistic approach to improving both individual and organisational performance.
In our Board, coaching interventions are always linked to organisational objectives whilst recognising the need for individuals to have support and challenge as part of the coaching process. Coaching is always a confidential and supportive intervention. It is well recognised that when managers take a coaching approach with staff that engagement, motivation and productivity can increase.
The Board has a small bank of professional trained coaches who are able to provide a coaching service. To access this coaching service you need to discuss your needs with your line manager in the first instance.
Executive Coaching
Executive coaching is a structured development approach where coach and ‘coachee’ undertake a series of one to one meetings to oversee a process of personal development.
Meetings are confidential and a coach will never share any details of what is discussed (unless helpful to the process and by agreement).
A register of approved executive coaches who have been chosen for their experience and results at this level is now in place.
Approved coaches have experience in different organisational settings, are professionally accredited and licensed to use a range of psychometrics and 360 tools if applicable.
Coaching activity will be time bound, regularly reviewed against objectives and evaluated by OD both at the individual level and as an overall provision in the organisation.
Further Information
To discuss whether coaching is the right option for you, or for further information please contact the OD Team.
Everything offered by OD aims to be inclusive for all staff. If we can help with any arrangements, for instance for staff with a sensory impairment, that would make our programmes or materials easier for you to access.
Leading Effective Teams
Teams are the vehicle that brings the skills, knowledge and experience of individuals together to enable NHS Greater Glasgow and Clyde be a highly effective organisation.
The Affina Team Journey provides a proactive approach for implementing and maintaining effective team working across the whole organisation and between organisations. Both underpin and reflect our organisational value “we work as one team”.
The Affina Team Journey is a unique step-by-step interactive programme, providing easy-to-use diagnostic tools for assessing a team’s performance, and tools to develop team effectiveness in the areas identified in research as essential for team success.
For further information contact the OD Team.
Everything offered by OD aims to be inclusive for all staff. If we can help with any arrangements, for instance for staff with a sensory impairment, that would make our programmes or materials easier for you to access.
Medical Management Programme
Introduction letter from Dr Jennifer Armstrong, Board Medical Director
Dear Colleague,
I am pleased to make you aware of and fully support you to take part in the Medical Management Development Programme in NHSGGC. This new initiative has been created to address the succession planning and development needs of doctors in leadership positions across primary, secondary and mental health care. As you know, these roles are critical for shaping clinical and service change across the Board, for the effective leadership and management of the medical workforce and ultimately for the delivery of high quality patient care. The programme aims to support your development in the skills and knowledge required in these roles and it also contributes to your continuous professional development.
There are 8 modules in the programme, all delivered three times a year in a published schedule across the calendar year. This gives you flexible options for attendance and completion of the programme over 12 months. There will also be opportunities for coaching and mentoring support and further learning.
If you are keen to advance your career in Medical Management or anticipate that you will be asked to fulfil such a position in the future please take full advantage of this important development opportunity.
Many thanks,
Dr Jennifer Armstrong, Board Medical Director
Information on all modules is available in our programme descriptor
PAGE AND MODULES BEING UPDATED.
Medical Management Programme Materials and Pre-Reading
Slides and pre-reading for each module (where available) are available on our Staffnet page
Everything offered by OD aims to be inclusive for all staff. If we can help with any arrangements, for instance for staff with a sensory impairment, that would make our programmes or materials easier for you to access.
Leadership Lift Foundations
The North, South and Clyde Sectors and Womens and Childrens Services have joined forces to collaborate on a pilot leadership programme called Leadership Lift Foundations (LLF).
Leadership Lift Foundations is a leadership development journey that focuses on practical application and group mentoring support alongside leadership and management theory. The desired outcome is that, as a leader, you feel proactively supported in your leadership role.
The programme runs over a 4 month period in short, bite sized sessions and starts with completion of a self-assessment questionnaire from which you will receive a leadership profile report, a profile debrief and a development planning session to enhance and align with your existing Personal Development Plan (PDP).
It includes leadership modules and modules related to operational management, including group mentoring and learning sessions aimed at reflecting and embedding lessons from the leadership and management modules which you complete and involves discussing practical application and case examples with experienced leaders to ensure the transfer and practical application of learning as well as expand your circle and network of support.
The programme will run collaboratively across GGC so that learning can be shared across and create opportunities for cross collaboration and networking, so you will get to meet other leaders from across the organisation.
To complete the programme will require approximately 14 days of your time over 4 months, at an average of 2 hours a week. All sessions will be virtual using MS Teams.
For more information contact the OD Team.
Mentoring Information
Was this helpful?
Thank you for supporting the NHS Greater Glasgow and Clyde COVID-19 Vaccination Programme, one of the Health Board’s largest vaccination programmes ever undertaken.
NHSGGC have received thousands of applications from individuals who are interested in becoming COVID-19 Vaccinators or COVID-19 Healthcare Support Worker Vaccinators. Applications for new individuals are currently suspended whilst the existing applications are processed.
Any future opportunities will be advertised on the NHS Scotland Recruitment website. Be sure to sign up for job alerts on the NHS Scotland Recruitment to receive notifications when NHS Greater Glasgow and Clyde are accepting more applications for COVID-19 Vaccinators or COVID-19 Healthcare Support Worker Vaccinators.
COVID-19 Vaccinator Eligibility
COVID-19 Vaccinators
To work as a COVID-19 Vaccinator, you must hold current registration in one of the eligible occupations:
- Nursing & Midwifery Council (NMC) – all occupations.
- General Medical Council (GMC) – all levels (excluding FY1 doctors).
- General Dental Council (GDC) – Dentist, Dental Hygienist, Dental Therapist.
- Health and Care Professions Council (HCPC) – Chiropodist / Podiatrist, Dietitian, Occupational Therapist, Orthoptist, Paramedic, Physiotherapist, Prosthetists / Orthotist, Radiographer, Speech and Language Therapist.
- General Pharmaceutical Council (GPhC) – Pharmacist.
- General Optical Council (GOC) – Optometrist.
CVOVID-19 Healthcare Support Worker Vaccinators
If you do not hold a current registration in one of the occupations listed above, you may be eligible to apply to work as a COVID-19 Healthcare Support Worker Vaccinator.
Rates of Reimbursement
COVID-19 Vaccinators
The rates of pay are guided by the Scottish Government. As of 04 March 2022, they are as follows:
- All COVID-19 Vaccinators, regardless of profession or experience, will be reimbursed on the Band 5 Agenda for Change payscale.
COVID-19 Healthcare Support Worker Vaccinators
All COVID-19 Vaccinator Healthcare Support Workers, regardless of profession or experience, will be reimbursed on the Band 3 Agenda for Change payscale.
Training Requirements
In conjunction with the Scottish Government, NHS Education for Scotland (NES) and pharmaceutical organisations, a wealth of training has been developed in a short space of time, in order to keep yourself and our patients safe. NHS Greater Glasgow and Clyde have developed a training schedule in which all COVID-19 Vaccinators and COVID-19 Healthcare Support Workers must demonstrate competence in.
The training schedule will be updated, as new vaccines are developed and the vaccination programme evolves.
- Training schedule for COVID-19 Vaccinators
- Training schedule for COVID-19 Healthcare Support Worker Vaccinators
As part of the COVID-vaccinator recruitment process, you will be asked to confirm (and provide evidence, where possible) that you meet the NHS Greater Glasgow and Clyde COVID-19 Vaccinator or COVID-19 Healthcare Support Worker Vaccinator training schedule.
Please note: Due to the sheer volume of applications received, there may be a delay in receiving your practical / induction training session. The NHS Greater Glasgow and Clyde Staff Bank are arranging training shifts as soon as spaces become available. We would like to thank you for your patience during this time.
Was this helpful?
Key Documents
Authorisation
Stage 1 Authorisation
All vacancies within NHS Greater Glasgow and Clyde (including vacancies within the Health and Social Care Partnerships).
The Vacancy Request Form must be authorised and signed by:
- Hiring Manager
- Head of Finance
- Service Director or Chief Officer
Stage 2 Authorisation
Some posts will require additional authorisation from senior officers within the Board. Please use the drop-down sections below to ascertain whether the vacancy requires additional (stage 2) authorisation.
Administrative services
New posts
In addition to the stage 1 approval process, these vacancies will require authorisation from the Financial Improvement Programme (FIP) Group. This group meets every Wednesday and further clarification may be sought on vacancy requests. The Vacancy Request Form (and accompanying documents) must be emailed to: recruitment.vacancies@ggc.scot.nhs.uk for the FIP Group’s consideration.
Replacement posts: Band 8A and above
In addition to the stage 1 approval process, these vacancies will require authorisation from the NHSGGC Chief Executive. The Vacancy Request Form (and accompanying documents) must be emailed to: vacancy.authorisation@ggc.scot.nhs.uk for the Chief Executive’s consideration.
If the post is jointly funded by the local authority, the post will also require authorisation from the Chief Executive of the local authority in addition to the Board’s Chief Executive.
Replacement posts: Band 2 – Band 7
No additional approval is required.
Allied Health Professions
New posts
In addition to the stage 1 approval process, these vacancies will require authorisation from the Financial Improvement Programme (FIP) Group. This group meets every Wednesday and further clarification may be sought on vacancy requests. The Vacancy Request Form (and accompanying documents) must be emailed to: recruitment.vacancies@ggc.scot.nhs.uk for the FIP Group’s consideration.
Replacement posts: Band 8A and above
In addition to the stage 1 approval process, these vacancies will require authorisation from the NHSGGC Chief Executive. The Vacancy Request Form (and accompanying documents) must be emailed to: vacancy.authorisation@ggc.scot.nhs.uk for the Chief Executive’s consideration.
If the post is jointly funded by the local authority, the post will also require authorisation from the Chief Executive of the local authority in addition to the Board’s Chief Executive.
Replacement posts: Band 2 – Band 7
No additional approval is required.
Executive Level
In addition to the stage 1 approval process, these vacancies will require authorisation from the NHSGGC Chief Executive. The Vacancy Request Form (and accompanying documents) must be emailed to: vacancy.authorisation@ggc.scot.nhs.uk for the Chief Executive’s consideration.
If the post is jointly funded by the local authority, the post will also require authorisation from the Chief Executive of the local authority in addition to the Board’s Chief Executive.
Health Science Services
New posts
In addition to the stage 1 approval process, these vacancies will require authorisation from the Financial Improvement Programme (FIP) Group. This group meets every Wednesday and further clarification may be sought on vacancy requests. The Vacancy Request Form (and accompanying documents) must be emailed to: recruitment.vacancies@ggc.scot.nhs.uk for the FIP Group’s consideration.
Replacement posts: Band 8A and above
In addition to the stage 1 approval process, these vacancies will require authorisation from the NHSGGC Chief Executive. The Vacancy Request Form (and accompanying documents) must be emailed to: vacancy.authorisation@ggc.scot.nhs.uk for the Chief Executive’s consideration.
If the post is jointly funded by the local authority, the post will also require authorisation from the Chief Executive of the local authority in addition to the Board’s Chief Executive.
Replacement posts: Band 2 – Band 7
No additional approval is required.
Medical and Dental
Consultant (replacement) positions
In addition to the stage 1 approval process, these vacancies will require authorisation from the Chief of Medicine within the relevant area.
Senior Medical positions and new Consultant posts
In addition to the stage 1 approval process, any new proposed: Consultant-level posts, Lead Clinician, Clinical Director, or Chiefs of Medicine posts will require authorisation from the NHSGGC Deputy Medical Director (Dr Scott Davidson).
The Vacancy Request Form (and accompanying documents) must be emailed to the Recruitment Service: Recruitment.Vacancies@ggc.scot.nhs.uk for authorisation.
Other Medical and Dental positions
No additional approval is required.
Medical and Dental Support
New posts
In addition to the stage 1 approval process, these vacancies will require authorisation from the Financial Improvement Programme (FIP) Group. This group meets every Wednesday and further clarification may be sought on vacancy requests. The Vacancy Request Form (and accompanying documents) must be emailed to: recruitment.vacancies@ggc.scot.nhs.uk for the FIP Group’s consideration.
Replacement posts: Band 8A and above
In addition to the stage 1 approval process, these vacancies will require authorisation from the NHSGGC Chief Executive. The Vacancy Request Form (and accompanying documents) must be emailed to: vacancy.authorisation@ggc.scot.nhs.uk for the Chief Executive’s consideration.
If the post is jointly funded by the local authority, the post will also require authorisation from the Chief Executive of the local authority in addition to the Board’s Chief Executive.
Replacement posts: Band 2 – Band 7
No additional approval is required.
Nursing and Midwifery
New posts
In addition to the stage 1 approval process, these vacancies will require authorisation from the Financial Improvement Programme (FIP) Group. This group meets every Wednesday and further clarification may be sought on vacancy requests. The Vacancy Request Form (and accompanying documents) must be emailed to: recruitment.vacancies@ggc.scot.nhs.uk for the FIP Group’s consideration.
Replacement posts: Band 8A and above
In addition to the stage 1 approval process, these vacancies will require authorisation from:
- The Chief Nurse (or equivalent) within the relevant area; and
- The NHSGGC Nursing Director Professor Angela Wallace. The Vacancy Request Form (and accompanying documents) must be emailed to: angela.wallace@ggc.scot.nhs.uk for the Nursing Director’s consideration; and
- The NHSGGC Chief Executive. The Vacancy Request Form (and accompanying documents) must be emailed to: vacancy.authorisation@ggc.scot.nhs.uk for the Chief Executive’s consideration.
If the post is jointly funded by the local authority, the post will also require authorisation from the Chief Executive of the local authority I addition to the Board’s Chief Executive.
Replacement posts: Band 6 and Band 7
In addition to the stage 1 approval process, these vacancies will require authorisation from the Chief Nurse (or equivalent) within the relevant area.
Replacement posts: Band 2 – Band 5
No additional approval is required.
Personal and Social Care
New posts
In addition to the stage 1 approval process, these vacancies will require authorisation from the Financial Improvement Programme (FIP) Group. This group meets every Wednesday and further clarification may be sought on vacancy requests. The Vacancy Request Form (and accompanying documents) must be emailed to: recruitment.vacancies@ggc.scot.nhs.uk for the FIP Group’s consideration.
Replacement posts: Band 8A and above
In addition to the stage 1 approval process, these vacancies will require authorisation from the NHSGGC Chief Executive. The Vacancy Request Form (and accompanying documents) must be emailed to: vacancy.authorisation@ggc.scot.nhs.uk for the Chief Executive’s consideration.
If the post is jointly funded by the local authority, the post will also require authorisation from the Chief Executive of the local authority in addition to the Board’s Chief Executive.
Replacement posts: Band 2 – Band 7
No additional approval is required.
Senior Managers
In addition to the stage 1 approval process, these vacancies will require authorisation from the NHSGGC Chief Executive. The Vacancy Request Form (and accompanying documents) must be emailed to: vacancy.authorisation@ggc.scot.nhs.uk for the Chief Executive’s consideration.
If the post is jointly funded by the local authority, the post will also require authorisation from the Chief Executive of the local authority in addition to the Board’s Chief Executive.
Support Services
New posts
In addition to the stage 1 approval process, these vacancies will require authorisation from the Financial Improvement Programme (FIP) Group. This group meets every Wednesday and further clarification may be sought on vacancy requests. The Vacancy Request Form (and accompanying documents) must be emailed to: recruitment.vacancies@ggc.scot.nhs.uk for the FIP Group’s consideration.
Replacement posts: Band 8A and above
In addition to the stage 1 approval process, these vacancies will require authorisation from the NHSGGC Chief Executive. The Vacancy Request Form (and accompanying documents) must be emailed to: vacancy.authorisation@ggc.scot.nhs.uk for the Chief Executive’s consideration.
If the post is jointly funded by the local authority, the post will also require authorisation from the Chief Executive of the local authority in addition to the Board’s Chief Executive.
Replacement posts: Band 2 – Band 7
No additional approval is required.
Therapeutic Services
New posts
In addition to the stage 1 approval process, these vacancies will require authorisation from the Financial Improvement Programme (FIP) Group. This group meets every Wednesday and further clarification may be sought on vacancy requests. The Vacancy Request Form (and accompanying documents) must be emailed to: recruitment.vacancies@ggc.scot.nhs.uk for the FIP Group’s consideration.
Replacement posts: Band 8A and above
In addition to the stage 1 approval process, these vacancies will require authorisation from the NHSGGC Chief Executive. The Vacancy Request Form (and accompanying documents) must be emailed to: vacancy.authorisation@ggc.scot.nhs.uk for the Chief Executive’s consideration.
If the post is jointly funded by the local authority, the post will also require authorisation from the Chief Executive of the local authority in addition to the Board’s Chief Executive.
Replacement posts: Band 2 – Band 7
No additional approval is required.
Was this helpful?
Your application form will play a key part in deciding whether you will be short listed for interview for the post you apply for. It is important that you take the time to complete it as fully and as accurately as possible.
Please read the guidance notes in the candidate information pack for the job carefully before you start. You should also read the Job Description/Person Specification for the post that you are applying for.
Before you submit your application please check that all of the relevant parts of the NHS Scotland Application form have been completed.
Application Form – Personal Details and Criminal Convictions Declaration
This section provides our Recruitment team with contact details and confirms your eligibility to work in the UK and requires the declaration of any criminal convictions for posts exempt from the Rehabilitation of Offenders Act.
Data Protection
Any data about you will be held in completely secure conditions, with access restricted to only those involved in the administration of the post have applied for.
Your Equalities Opportunities Monitoring information will not be accessible to anyone involved in the shortlisting/interview process.
It will be understood that by submitting the application form you are giving your consent to the processing of your data in the ways described above.
Eligibility
It a criminal offence for any employer to hire a new employee whose immigration status prevents him or her from legally working in the UK.
This applies to all types of NHS employment, including part-time, temporary or bank posts. All applicants, regardless of nationality, will be asked to produce evidence of eligibility to work in the UK and these will be verified at interview and again should you be successful for a post. More information about immigration and the sponsorship process can be found at the UK Government website.
Application Form – Employment Details
You must give us details of your current or most recent employer.
Please provide details of previous employment including part-time, temporary, clinical attachments, honorary posts or voluntary work.
Qualifications and Training Details
Please provide details of all relevant education, qualifications & training courses. You should expect to provide copies of relevant qualifications in the event that you are offered a post.
Assessment Form A – Questions
Applicants who can demonstrate that they possess the knowledge, skills, experience, and clinical competencies required for the job give themselves the best opportunity of being shortlisted and selected for interview.
Make sure you review the job description/person specification for the post that you are applying for as that will detail the skills, abilities, clinical competencies and experience required for the post.
It is important to provide evidence that you can meet each of the requirements in the job description/person specification, by giving specific examples of what you have done and how you believe you meet each requirement. Remember the person reviewing your application form won’t be able to second guess your skills and experience unless you outline it. Unless you provide evidence that you possess all the requirements, supported by relevant examples, you may not be included in the shortlist.
Your application will be considered by a Clinician(s), who will decide who to select for interview on the basis of the essential criteria for the post. It is important, therefore, that you work on your application to ensure it reflects the job description and the recruitment advertisement.
Remember to be accurate and honest when you complete your application as the information you provide will be verified at various stages of our recruitment and selection process.
Referees
If you are shortlisted for interview, our Medical Recruitment Team will contact your referees. Satisfactory references must be received to an acceptable standard before any new employee can commence employment. If you are in employment, or have been in employment, please make sure that at least one of the referees you nominate includes your present or most recent employer and should be your Line Manager/Educational Supervisor/Clinical Lead. We do not accept referees from family members or friends.
Please ensure you provide accurate contact details including an e-mail address for your referees and most importantly don’t forget to get their permission to be contacted by us.
The Selection Process & Shortlisting Stage
Upon submission of your application, you will receive a notification that it has been received and awaits the process of shortlisting. Shortly thereafter, you will either be invited to select an interview slot or, if you have been unsuccessful at the shortlisting stage, you will be notified by email that your application has failed shortlisting.
Interview Stage
If you are selected for interview, you will be asked to attend a panel interview either in person or via Microsoft Teams. In addition to a set of interview questions, candidates may be asked to deliver a presentation, or provide a response to a clinical scenario. Candidates will be advised in advance of the interview what they will be expected to do on the day, so will have time to prepare.
You will be asked to bring the following original documents to interview: Passport, biometric card (where appropriate,) Medical Degree Certificate, GMC Certificate or letter, and 2 utility bills to confirm your address.
Equal Opportunities and Equality Monitoring
NHS Greater Glasgow and Clyde’s staff are our most valuable resource. By ensuring we have good recruitment practice that will make a significant contribution to ensuring we promotes a culture of person-centred care, placing the patient at the heart of everything we do.
We are committed to attracting the highest calibre of job applicants through a fair and consistent recruitment process, treating all our candidates fairly to ensure we recruit the best person for each vacancy.
We endeavour to ensure we do not discriminate during any stage of the recruitment process and in particular comply with the Equality Act 2010 which makes it illegal to discriminate against protected characteristics i.e. age, disability, sex, gender reassignment, marriage or civil partnership, pregnancy and maternity, race, religion or belief, sexual orientation.
We are required to gather data for both applicants and employees to ensure that our policy on Equality and Diversity is effective and meets statutory requirements. All applicants are therefore required to provide the information requested in the Application Form’s Declarations section – this information is not made available to the shortlister(s). .
Finally we hope you find the guidance we have provided useful and we wish you good luck if you decide to apply for a post at NHS Greater Glasgow and Clyde.
NHS Greater Glasgow and Clyde participates in 2 schemes aimed at supporting the employment and career development of disabled people :
Job Interview Guarantee (JIG) scheme means that if a candidate declares a disability , and meet the minimum/essential criteria outlined within the Person Specification for the post then they will be guaranteed an interview.
Job Centre Plus Two Ticks symbol: the two ticks scheme is a recognition given to NHS Greater Glasgow and Clyde by Jobcentre Plus because we have agreed to take action to meet five commitments regarding the employment, retention, training and career development of disabled employees. It is represented by the two ticks disability symbol (displayed right) that participating organisations in the UK are authorised to display. As a symbol user, an interview is guaranteed to any candidate with a disability whose application meets all of the minimum/essential criteria for the post.
Pre-Employment Checks
Disclosure of Criminal Convictions
- Rehabilitation of Offenders Act 1974 (Exclusions and Exceptions) (Scotland) Order 2013
- The Protection of Vulnerable Groups (Scotland Act ) 2007 The 1997 Police Act
Criminal Convictions – Rehabilitation of Offenders Act 1974
NHS Scotland is exempt from the 1974 Rehabilitation of Offenders Act (Exclusions & Exceptions) (Scotland) Amendment Order 2015. This means that unless stated in the job description, person specification or application pack, you must tell us about any previous unspent convictions along with only those spent convictions that relate to Disclosure Scotland’s ‘Offences which must always be disclosed’ list. If you are offered employment, any failure to disclose such convictions could result in withdrawal of the offer of employment dismissal or disciplinary action. Any information you give will be considered only in relation to the post for which the application you submit refers to.
Information will be verified by Disclosure Scotland for relevant posts.
Please note; you are not required to tell us about any previous spent convictions that relate to Disclosure Scotland’s ‘Offences which are disclosed subject to the rules’ list.
Please refer to Disclosure Scotland’s website for further guidance and details on the two lists relating to spent convictions.
Certificate of Good Standing
If you have been living out with the UK for a period of more than a year within the last 5 years, you will require to submit a Certificate of Good Standing from the police authority in that country.
General Medical Council (GMC)
To be eligible to practice medicine in the UK, you will require a licence to practice through the General Medical Council. If you are applying for a substantive Consultant post, you will require to be on the specialist register for your particular specialty. You can find out more on the GMC and specialist registration website.
Revalidation
All doctors who do not have a National Training Number require to undergo revalidation, this includes all non-training career grade doctors in secondary care who have a substantive, locum or honorary contract with NHS Greater Glasgow and Clyde. It does not include doctors in training (including Foundation Year trainees, Specialty Registrars, Core Trainees and those who hold Locum Appointment for Training posts), for whom NHS Education for Scotland (NES) is the body responsible for revalidation.
NHS Greater Glasgow and Clyde Responsible Officers are as follows:
Responsible Officer: Dr Jennifer Armstrong, Medical Director
Please note: General Practitioners (GPs) who carry out the majority of their clinical work within Secondary Care should undertake a single appraisal within Secondary Care, which also covers their Primary Care practice. All GPs are required to work an average of fifty sessions per year to demonstrate that they are maintaining their clinical skills.
If you have a specific query or question regarding Medical Revalidation or Appraisal please email medical.revalidation@ggc.scot.nhs.ukand a member of the Medical Staffing Team will get back to you.
Doctors in training with queries regarding revalidation should contact NES for clarification: trainingcontacts@nes.scot.nhs.uk.
Consultant Posts: Certificate of Completion of Training – Criteria for Interview
To be interviewed for a substantive Consultant post, those trained in the UK should have evidence of higher specialist training leading to CCT and be within 6 months of confirmed entry from date of interview or have been awarded Specialist Registration via the Certificate of Eligibility for Specialist Registration (CESR) . Non-UK applicants must demonstrate equivalent training.
Criteria before taking up post
Before commencement in a Consultant post you require to be on the GMC Specialist Register for the relevant Specialty or the GDC Specialist List for the relevant Specialty.
Was this helpful?
Guidance on Consultant Appointments
Consultant Appointments must be carried out in accordance with the Scottish Government’s General Guidance on Medical & Dental Appointments
Overarching Principles for Consultant Recruitment within NHS in Scotland:
- The consultant recruitment process is owned and determined by the Health Board as the employer.
- The management of and decisions taken regarding the consultant recruitment process is the responsibility of the Health Board.
- It is recognised that externality provides a valuable contribution to the objective assessment of applicants and the role of an External Adviser is included within this consultant recruitment process
Summary Guide
Consultants carry ultimate clinical responsibility for every patient seen under their care. The public is therefore entitled to expect that all consultants will have reached the highest standards of skill and knowledge and this is guaranteed by means of a statutory appointments procedure for recruitment of consultants laid down in regulations. The regulations and supporting guidance were revised in July 2009 (The National Health Service (Appointment of Consultants) (Scotland) Regulations 2009).
While the majority of the actions within the consultant recruitment process, which were previously subject to regulation, now lie with the NHS boards who hold responsibility for the process, some key elements are still subject to regulation and remain under statutory control.
The statutory element includes the appointment of a trained External Adviser from a different NHS board as a full member of the consultant assessment panel: this is intended to ensure the clinical quality of appointed candidates is maintained. The External Adviser will have been trained in selection processes and, with experience of other appointments, can provide advice on the appointment from a different perspective than the local clinical team.
Key Roles within the Recruitment Process
Within the recruitment process it is for the recruiting Board to determine the staff and their roles within the process; however each recruitment process should include the following key roles:
The Board Lead Officer
The Board should identify a Lead Officer to manage an individual recruitment process with support from the HR department. Within the recruitment process it is anticipated that this Lead Officer will often be a medical manager or dental manager, who may, depending on the size of the Board, or the specialty involved, choose to either directly lead the recruitment process or identify who will. Other possibilities for this role include a lead clinician from within the service or the clinical service manager.
Chair
The Chair of the panel has delegated authority from the recruiting Board to make an offer of employment. This authority is contained within the regulations. Boards may choose to appoint the Lead Officer as Chair, or may alternatively choose a senior manager or non-executive director to chair the assessment panel.
External Adviser
The regulations require a single External Adviser is included on the assessment panel for consultant appointments within NHS in Scotland. The role of the External Adviser will be to advise the recruiting Board on each stage in the process, including commenting and advising on the job description, person specification, the selection methodology and participating in the selection process. This External Adviser is identified from the list of External Advisers maintained by the Academy, and must be external, i.e. not employed by the recruiting Board, and must be in the same specialty as the post being appointed to. In rare instances of small specialties it may be necessary to seek an External Adviser from out with Scotland.
The Assessment Panel
The assessment panel is convened by the Board to conduct the candidate assessment. Within this recruitment process, as the Boards determine the selection methodology for appointing to consultant posts, the Assessment Panel is also to be determined by the recruiting Board to best support and facilitate the methodology chosen to assess the suitability of candidates. This assessment may include profiling, aptitude tests or multi-station interviews. The panel must include at least one consultant from the specialty. Where possible that consultant should be from the employing Board.
Depending on the nature of the post and the extent of any undergraduate teaching or training duties the Board may include University representation on the assessment panel and requests for University representatives should be submitted to the Dean.
While there is no set limit on the size of the panel, under the regulations it remains that the panel must include a Chair, with delegated authority from the Board, an External Adviser as outlined above and one other consultant from the specialty
Planning and Advertising a Consultant Post
When recruiting to posts it is advised that the planning for a consultant appointment begins well before the post is to be filled. Consideration should be given to service needs, the amount and level of training that may be required, teaching, supervision of junior staff, continuing professional development, research and any special interests and produce a draft job description and person specification which must be sent to the External Adviser for their advice and comment.
All potential applicants should have access to the job description; the person specification; information from the board with details of arrangements for practice, e.g. units, clinics etc; details of staffing and relevant services covered; where appropriate, information about undergraduate or postgraduate medical/dental teaching; and the relevant TCS including pay. A Job Plan must also be available for the consideration of candidates for appointment to a consultant post.
We must ensure that we look to advertise details of vacant posts widely which will include the use of the NHS Scotland online job portal www.jobs.scot.nhs.uk , medicaljobs.scot.nhs.uk and where necessary other online professional job portals and journals e.g. BMJ ( British Medical Journal ) .
Eligibility for appointment and specialist register
On successful completion of specialty training, doctors are awarded a certificate of completion of training (CCT), allowing them to practice across Europe as recognised ‘specialists’. The GMC recommends CCT holders for inclusion on the specialist register, which it administers. The specialist register includes the names of all CCT holders together with those of other eligible specialists, and shows their specialty and, if requested, any particular field of expertise within it. Eligible specialists are defined as:
- European Economic Area nationals holding recognised specialist qualifications
- Overseas nationals holding specialist qualifications that are deemed equivalent to the CCT
- Doctors who have followed academic or research training paths, resulting in a level of knowledge and skill consistent with NHS consultant practice in that specialty.
From 1 January 1997 it has been a legal requirement for all doctors to be on the GMC’s specialist register before they can take up a consultant appointment.
In the case of consultant dental posts, individuals must be a registered dental practitioner or a fully registered medical practitioner. However, trainees may explore the possibility of post-CCT careers as soon as it is apparent that a CCT will be awarded in the near future. Consequently, SpRs and StRs are able to apply for a Consultant appointment provided the expected date of award of their CCT (or recognised equivalent, if outside the UK) falls no more than six months after the date of interview for the consultant post. The consultant assessment panel must also be satisfied that the applicant is sufficiently near to the completion of training to enable them to judge the applicant’s suitability for a consultant post.
Membership of the Assessment Panel
The assessment panel is convened by the appointing board to conduct the candidate assessment. This assessment may include profiling, aptitude tests or multi-station interviews. The panel must include at least one consultant from the specialty. Where possible that consultant should be from the employing board. Depending on the nature of the post and the extent of any undergraduate teaching or training duties, the board may include university representation on the assessment panel. While there is no set limit on the size of the panel, under the regulations the panel must as a minimum include a Chair, with delegated authority from the Board, an External Adviser and one other consultant from the specialty.
External Adviser
The regulations require that a single External Adviser is included on the assessment panel for consultant appointments within the NHS in Scotland. The role of the External Adviser is to advise the recruiting board on each stage in the process, including commenting and advising on the job description, person specification, the selection methodology and participating in the selection process. This External Adviser is identified from the list of External Advisers maintained by the Academy of Royal Colleges and Faculties in Scotland, and must be external i.e. not employed by the recruiting board, and must be in the same specialty as the post being appointed to. In rare instances of small specialties it may be necessary to seek an External Adviser from outside Scotland.
All newly appointed External Advisers undergo training before they are included on the adviser list, and if reappointed to the list again, should undergo refresher training.
This training is coordinated by NHS Education for Scotland and includes:
- detailed training on equality and diversity issues;
- refreshers on specialty training curricula and assessment methods used;
- updates on selection methodology and tools that have been used successfully;
- the option to shadow an External Adviser and observe the process, although it should be emphasised that observers will play no role in the recruitment process.
Process
Under the regulations, recruiting boards will appoint a Chair for the assessment panel. The Chair will hold delegated authority to offer the post on behalf of the board once the panel has considered the candidates.
Boards should draw up a policy on the use of visits as part of the employment process and communicate this policy to all applicants. Visits are intended to inform the applicant regarding the department and the requirements of the post. Depending on the nature of the post the policy on visits should look to offer applicants an opportunity to visit the department and meet with key staff. The option of a visit, and the timing of such a visit, should be determined by the board, and should be made available to all applicants at the same point in the recruitment process.
Once the assessment panel has made a decision on which candidate(s), if any, should be offered the post, the Chair and the Recruitment Service will then take responsibility for offering and contracting with successful candidates .
All members of the assessment panel hold equal responsibility for raising concerns at any stage within the recruitment process with the Chair. In these instances, it is for the Chair to assess these concerns and to determine whether or not to proceed with the recruitment process. If the decision is taken to proceed to appointment, the Chair should note the concerns raised and indicate the basis on which the decision to proceed was taken. If the Chair decides not to proceed, this decision is reported back to the board, outlining the basis on which this decision was taken. It is for the board to decide on next steps and whether to re-run the process.
For more information visit :
Was this helpful?
This section provides links to documents and process will support you across all stages of the recruitment process.
Completing the application form and the Recruitment process
Completing the Application Form
Your application form will play a key part in deciding whether you will be shortlisted for interview. It is important that you take the time to read the advert and the job description/person specification for the post and complete the application form fully and as accurately as possible.
Applications are made online through the NHS Scotland job site. When you click the ‘Apply for job’ button on the advert, you will be asked to create an account using an email address or social media account. For returning candidates, you you can copy from a previous application or create a new one. If you prefer to copy, make sure that you go through each section to ensure that the information is complete and up-to-date.
The system will timeout after 30 minutes of inactivity so please save your application regularly. You can save your progress and come back later if you wish, just remember your password so you can log back in.
Please note:
- Remember to review your application prior to submission as you will not be able to make changes once you submit the form.
- Be accurate and honest on your application form as the information you provide will be verified at various stages of our recruitment and selection process .
- Your email and contact telephone number must be correct as these will be used to contact you. The primary method of contact for all updates is via email.
- Some recruitment may include initial screening questions to verify that you meet the requirements for the job e.g. UK Professional registration
- Curriculum vitae (CVs) will NOT be accepted as part of the application process unless you are applying for a Medical Staffing (Doctor, Consultant etc) Position
- The Job reference number is an important information to take note of as this is the unique ID of the post. This will allow us to identify which post is being referred to.
- You should save an electronic copy of the advert, job description/person specification, and the candidate pack for future reference
- On the Assessment section, you may find it helpful to prepare your answers in a separate document and copy and paste your answers into the online form. You will also be asked to provide your National insurance number on this section.
- All adverts close at midnight on the closing date unless otherwise stated. Please submit your application as soon as possible. If any updates on the closing date occur, you will be contacted via email.
- You can check the status of your application by checking your account online.
- If you delete your application, you will not be able to re-apply.
Eligibility to Work in the UK
It is a criminal offence for any employer to hire a new employee whose immigration status prevents him or her from legally working in the UK in the post they have applied for. This applies also to all types of NHS employment, including part-time, temporary or bank posts. All applicants regardless of nationality will be asked to produce evidence of eligibility to work in the UK as part of the application process specifically at the interview and pre-employment checks stages.
Please complete the relevant sections as accurately as possible on the application form, providing the type of right to work in the UK (RTW UK) visa that you hold as well as the expiry date, if applicable.
Applications from job seekers who require a RTW will be considered alongside all other applications subject to meeting the essential criteria as detailed in the Job Description and Person Specification for the post. Before making your application, you should check the eligibility criteria for UK Visa and Immigration
Qualifications and Training Details
Please provide details of all relevant education, qualifications and training courses.
Specific requirements such as registration/membership details to a Professional Regulatory Bodies such as the Nursing and Midwifery Council (NMC) or General Medical Council (GMC), must be provided if relevant to the vacancy
Employment information
For the Employment section, please start with your current/most recent employer and work back through your employment history. Please also include any part-time or temporary jobs, work placements, volunteering roles, or any career breaks
(student/parent/carer/etc.)
Referees
You must provide at least two (2) referees are required which must cover the past three (3) years and must include your present or most recent employer. We do not accept references from family members or friends.
If you are appointed to the post you have applied for, our Recruitment Team will contact your referees. Satisfactory references must be received to an acceptable standard before any new NHS Greater Glasgow and Clyde employee can start work for us.
Please ensure that you provide accurate contact details including an e-mail address for your referees and, most importantly, don’t forget to get their permission to be contacted by us.
Please refer to Disclosure Scotland’s website for further guidance and details on the two lists relating to spent convictions.
Statement in Support of Your Application
Applicants who can demonstrate in their application that they possess the knowledge, skills, experience and abilities required for the job give themselves the best opportunity of being shortlisted and selected for interview.
You can use this section to provide evidence that you can meet each of the requirements in the job description/person specification, by giving specific examples of what you have done and how you believe you meet each requirement. Remember that the person reviewing your application form won’t be able to second guess your skills and experience unless you outline it.
A good tip is to use the selection criteria in job description/person specification as headings in the order that they have been listed, to make sure that you address them especially the ones under the Essential Criteria.
Declaration
Before submitting your application, please make sure that you read this section as it will highlight any parts of the form which haven’t been completed and it also covers the following important information:
- Criminal Convictions Declaration – NHS Scotland is exempt from the 1974 Rehabilitation of Offenders Act (Exclusions & Exceptions) (Scotland) Order 2003.
- Accuracy of Information – False or misleading information can causE disqualification of the application and dismissal from employment if appointed to the post.
- General Data Protection Regulation (GDPR) and Data Protection Act 2018 – Your data will be stored by Jobtrain and will be used only by NHSGGC authorised staff for the purpose of processing your job application, making recruitment decisions and for statistical and audit purposes. It will be retained, archived, and deleted in line with the NHS Scotland retention policy and will not be passed to any third party organisations without your permission
Equal Opportunities and Equality Monitoring
NHS Greater Glasgow and Clyde participates in 2 schemes aimed at supporting the employment and career development of disabled people :
Job Interview Guarantee (JIG) scheme: if a candidate declares a disability, and meets all the minimum/essential criteria outlined within the Job description/Person specification for the post then they will be guaranteed an interview.
Job Centre Plus Two Ticks symbol: the two ticks scheme is a recognition given to NHS Greater Glasgow and Clyde by Jobcentre Plus in meeting the five commitments regarding the employment, retention, training and career development of disabled employees. As a symbol user, an interview is guaranteed to any candidate with a disability whose application meets all of the minimum/essential criteria for the post.
NHSGGC is committed to applying and promoting best employment equality practice in it efforts to eliminate discrimination and create working environments where all our staff, patients, relatives, visitors and carers are treated fairly and with respect.
We always endeavour to not discriminate during any stage of the recruitment process and in particular comply with the Equality Act 2010 which makes it illegal to discriminate against protected characteristics i.e. age, disability, sex, gender reassignment, marriage or civil partnership, pregnancy and maternity, race, religion or belief, sexual orientation.
We are required to gather data for both applicants and employees to ensure that our policy on Equality and Diversity is effective and meets statutory requirements. The Equal opportunities monitoring form is recorded separately from your application form and can only be accessed by the Recruitment team. All recruitment documentation for unsuccessful applicants are confidentially destroyed after 12 months.
When completing the Equal Opportunities section of the online application form, you can use this section to inform us if you will require any special arrangements for the interview e.g. Wheelchair access, induction loop, etc
Criminal Convictions
- Disclosure of Criminal Convictions
- Rehabilitation of Offenders Act 1974 (Exclusions and Exceptions) (Scotland) Order 2013
- The Protection of Vulnerable Groups (Scotland Act ) 2007 The 1997 Police Act
- Criminal Convictions – Rehabilitation of Offenders Act 1974
NHS Scotland is exempt from the 1974 Rehabilitation of Offenders Act (Exclusions & Exceptions) (Scotland) Amendment Order 2015. This means that unless stated in the job description, person specification or application pack, you must tell us about any previous unspent convictions along with only those spent convictions that relate to Disclosure Scotland’s ‘Offences which must always be disclosed’ list. If you are offered employment, any failure to disclose such convictions could result in withdrawal of the offer of employment dismissal or disciplinary action. Any information you give will be considered only in relation to the post for which the application you submit refers to.
Information will be verified by Disclosure Scotland for relevant posts.
Please note, you are NOT REQUIRED to tell us about any previous spent convictions that relate to Disclosure Scotland’s ‘Offences which are disclosed subject to the rules’ list.
Recruitment stages
Shortlisting Stage
The NHS Greater Glasgow and Clyde Selection panel (Panel), which includes as a minimum two (2) members of staff [one of which is always the hiring /line manager for the post] will decide who to select for interview on the basis of the job description/person specification. These documents lists those qualities e.g. skills, knowledge, experience, qualifications etc, which are ‘essential’ i.e. which you must have to do the job, and those which are ‘desirable’ i.e. which will help somebody to perform the complete range of tasks in the job more readily. It is important, therefore, that you work on your application to ensure it reflects the person specification, the job description and the recruitment advertisement.
At shortlisting stage, applications forms are anonymised and only the information about Education, Employment, and Supporting statement are accessible to the Panel. This helps ensure that the shortlisting is fair and consistent and is based on the candidate’s skills, knowledge, qualifications, and experience.
Once shortlisting is complete, invitations for interview are sent to the selected candidates by our Recruitment Team.
Interview Stage
The interview format will depend on the post being recruited to, and can either be face-to-face or via MS Teams video. You will be requested to bring to the interview the originals of any relevant qualifications/certificates/awards that you hold and documents to verify your identification such as a photo identification.
In addition to a set of interview questions, candidates may be asked to deliver a presentation, sit a technical/skills test, or provide a response to a work based scenario. Candidates will be advised in advance of the interview what they will be expected to do on the day.
An interview panel is normally between 2-4 people depending on the post and will be more senior to the grade of the post being recruited to. It can also include panel members, external to NHSGGC, where appropriate to the post.
If you are invited to an interview you will receive an email requesting you to select a suitable date/time slot. If the interview is via MS Teams, you will also receive an email with the link to join.
Pre-Employment Checks
If you are invited for interview and are successful in being offered a job, after your interview you will receive via the Jobtrain system what is referred to as a Conditional Offer of Employment. At this stage you are the Preferred Candidate. Please note
you should not hand in your notice to your current employer at this stage.
The standard pre-employment checks cover the following aspects:
- A 2nd Stage Application Declaration
- An Identity Check Document verification appointment, in person, at the NHSGGC Recruitment Department. This will also include a Right to Work in the UK check. Our Recruitment team will advise on the arrangements for this stage.
- Qualifications & Professional Registration/Membership of NHS Regulatory Bodies check if applicable
- Reference Checks
- Occupational Health Check
- Driving licence, only if required for the purpose of carrying out the duties of the job
- Where applicable to the post, successful applicants will be subject to Disclosure Scotland’s Protection of Vulnerable Group (PVG) Scheme membership /Standard Disclosure checks to check their criminal convictions history and to ensure that they are not included on Barred Lists which prohibits them from working with vulnerable adults and children.
Application Stage FAQs
Where can I find a list of your vacancies?
Visit the NHS Scotland job portal or visit the NHSGGC Recruitment homepage.
You can sign-up for job alerts for roles that you are interested in.
How Often do you update your vacancies?
A new list of posts opens every Friday.
How can I apply for your jobs?
NHS Greater Glasgow and Clyde operates an Online Application Form system. You can apply directly for the vacancy of your choice on the NHS Scotland Jobs Website.
I have a CV why do I still need to complete an application form?
The application process is anonymous and decisions to shortlist candidates for interview are made ONLY on the contents of your application form.
If you do not provide all the information requested on the application form, it will not be evident that you meet the criteria listed in the job description and you will not be shortlisted for interview.
Please ensure that you read the job description carefully, complete all applicable sections of the application and ensure that your statement in support of your application clearly demonstrates how you meet the requirements of the post.
Please note Curriculum Vitae will NOT be accepted as part of the application process unless you are applying for a Medical Staffing (Doctor, Consultant etc) Position.
Can I still apply after the closing date?
Once the closing date has passed you cannot apply for a post. Applications must submitted by midnight on the closing date.
For any post closing earlier than midnight, the submission time will be clearly displayed in the advert on the SHOW site.
We highly recommend that you submit your application as soon as possible as some posts might close earlier than scheduled if it has received a high volume of response.
What do I do if I experience any difficulties submitting the application?
For any login issues or problems submitting applications, please contact the Jobtrain Jobseeker support hub in the first instance:
(online) Submit a ticket : Jobseeker Support Hub (jobtrain.co.uk) or
(phone) (+44)0161-850-2004 Monday-Friday 09:00-17:30 UK local time
How will I know you have received my application form?
You will receive notification from the NHS Scotland Jobs Website once your application has been successfully submitted.
When will I find our if i have been shortlisted for an interview?
All our posts are shortlisted within six weeks of the closing date. If you have not been contacted after six weeks it is unlikely that you have been shortlisted.
How do I find out if I have been shortlisted for an interview?
We will contact you via email with the invite to book your interview slot as well as any important information i.e. MS Teams video link, documents to bring etc
If I have not been shortlisted for an interview can you tell me why?
Yes. If you have not received an invitation to interview after 6 weeks from the closing, please email the Recruitment Team at nhsggcrecruitment@nhs.net quoting the job reference number and someone will contact you.
Interview Stage FAQs
I have not received an invitation to interview
If you have not received an invitation to interview by 6 weeks from the closing date of the post you have applied for, you should assume your application has been unsuccessful.
How should I prepare for my interview?
We understand that interviews can be a stressful experience for candidates but a little advance preparation will ensure you perform to the best of your ability on the day.
- Take note of the details of your interview- Video or face-to-face, location, date, time etc. Do you have the link to the video interview and does it work on your equipment? Do you know how to contact the Panel in case your are having technical issues or running late?
- Ensure that you have assembled all the documentation (see question 4 below) that you have been asked to bring to interview
- You can visit the NHSGGC website for more general information about NHS Greater Glasgow and Clyde and search for specific information about the department that you have applied to work with.
- Take the time to re-read your job description and how you will meet the requirements of the role.
- Prepare examples from your experience and practice your answers. For competency-based questions, it will help if you structure your answer using STAR (Situation/Task(goal), Action taken, Result)
- Give yourself plenty of time to arrive or be set-up (video interview)
What should I expect?
Interview techniques will vary but as a standard you should expect to be asked questions on the following;
- Confirmation of your identity and to produce supporting documentation
- Confirmation of you Right to Work in the UK and Supporting documentation
- Questions to test your ability to meet the requirements of the role based on the job description
- Questions to confirm how you meet the minimum essential and other criteria specified in the job description
- General questions based on the content of your application form.
What do I need to bring to the interview?
We are required to verify the Identity and Right to Work in the UK of all our applicants regardless of nationality.
It is essential that you bring confirmation of your identity, your Right to Work in the UK, evidence of qualifications if required by the job description and any professional registration/membership if required by the job description to interview.
I have been told I am the “Preferred Candidate” – What happens next?
Please keep reading below to view the Preferred Candidate FAQs.
I have been unsuccessful following the interview. Can I receive Feedback?
Yes. You can contact the Panel member named in your correspondence or you can email the Recruitment Team at nhsggcrecruitment@nhs.net, quoting the job reference number.
Preferred Candidate FAQs
I have been told I am the “Preferred Candidate” – What happens next?
All our offers are subject to satisfactory Pre-employment checks noted above under Recruitment stages- Pre-employment checks section above.
You will receive a Preferred Candidate Email after you have received the verbal offer from the Hiring manager, outlining the next steps.
Pre-employment checks take time and cannot start and be completed without your participation
If you are external to NHS GGC or if it is required for the post, you will receive an electronic link to your Occupational health questionnaire. Please complete this asap as the link expires after a couple of days. Completed forms are forwarded to the NHS GGC Occupational health team for processing. They might get in touch if they require more information.
Please contact your referees to advise them that we will be contacting them and request the prompt return of your reference.
Please do not hand in your notice until all your pre-employment checks are cleared.
Posts that require PVG Scheme Membership or Disclosure Scotland Check
- If required for your post, a PVG checks needs to be conducted. If you already hold a PVG Scheme membership, please ensure that you notify us, together with the type of membership that you hold i.e. for adults, for children, or for both.
- PVG forms are sent electronically via an email link from Recruitment. Please complete this form as soon as possible. Completed forms are forwarded automatically to Disclosure Scotland for processing.
- More information on Disclosure Scotland.
How long will the process take as my current manager is looking for an indication of when I will be handing my notice in?
This will depend on you completing and returning the appropriate paperwork required and the relevant appointments. How quick your reference forms come back will also come into play as well as how proactive the Hiring manager is in completing the outstanding actions on the system. For example, reviewing the checks, updating the online forms with reporting details etc
When should I hand in my notice in current employment?
When your new manager approves the pre-employment checks, they will phone you to agree a start date. You can now hand in your notice with this verbal confirmation which recruitment will follow up in writing.
Any queries that you might have regarding the role, please speak to the Hiring manager in the first instance.
I am internal and have shown ID at my interview, do I require to send further copies?
For interview purposes the panel require to confirm you are the person they are interviewing, for audit purposes we require a copy for your personal file.
Contact Us
Our office hours are 9.00am to 5.00pm Monday to Friday.
You can contact us by email at nhsggc.recruitment@nhs.scot or Call 0141 278 2700 (please listen to all the options and select the appropriate line)
Our Address is:
NHS Greater Glasgow and Clyde
Recruitment Service
Gartnavel Royal Hospital
Administration Building
1055 Great Western Road
Glasgow
G12 0XH
