Overall Winner – The Champions Board
Overall Winner Nominees
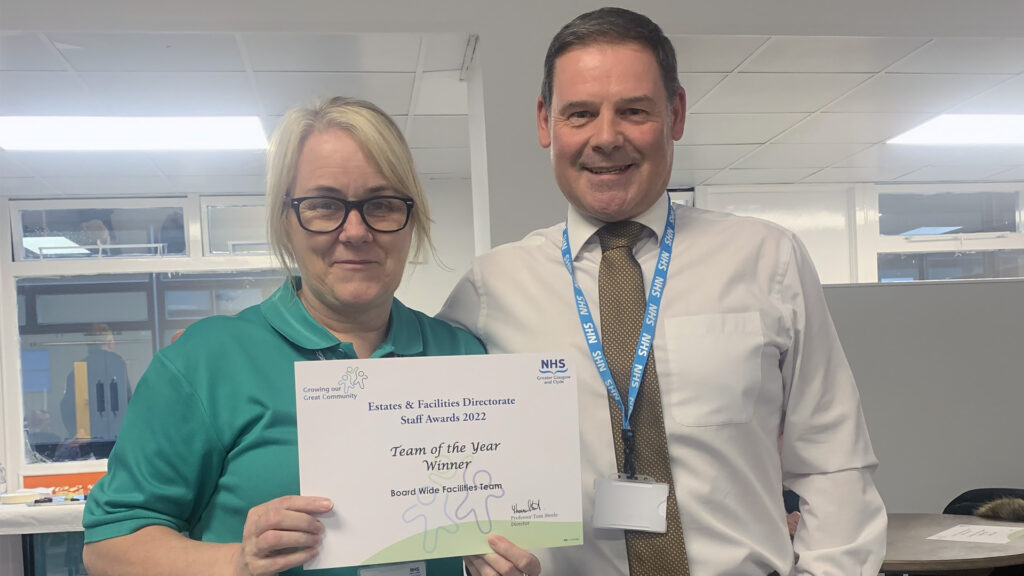
Team of the Year
Justice Services unpaid work Team and Children & Family Community Support Joint Initiative
The aims and objectives of this collaborative working is to ensure that our most vulnerable children and young people receive Christmas presents and food. Christmas can often be the hardest time of year for families who have on-going difficulties including but not exclusively financial hardship, addictions and domestic abuse.
The planning starts early around August time to engage with community groups about giving gifts. Most of the donations are collected by the Community Pay Back teams then sorted into individual gift bags for children of different age groups ready to be delivered to our vulnerable families and groups within our EDC communities.
Around 4000 individual gifts are distributed throughout the Community
Employee of the Year – Joint Winners
Justin Dott
Justin is a nurse in the ADRS; in his nomination is a report from a service user’s family:
“The second most valuable resource we found was Justin. He really engaged with our loved one and has guided him through recovery and relapse and continuing on to recovery again. Justin really understands the mental health aspects of the condition and he is sensitive to the needs of family members to be involved in the journey”.
Rab Kerr
Rab is a Social Work Justice Assistant with the Criminal Justice Social Work Team. He has been described as critical team player, being there for other staff and working well with Clients.
It is evidenced that he has been able to make “Real change with some of the most difficult and volatile clients in the manner that in which he has engaged clients and broken down barriers”.
Leader of the Year
Lorna Deazeley
Lorna has shown her leadership skills in the past 12 months as Senior Addiction worker. Lorna has developed close links with the homeless services providing outreach clinics at First Stop. This has enabled vulnerable homeless people to easily access support with alcohol and drug use. Lorna has provided Naloxone training to ADRS, Justice Services, homeless services and families affected by their loved ones drug use. Lorna has been a key member of the team supporting colleagues and building an effective relationship with both services and services users enabling them to Trust and accept support from services.
Innovation of the Year
East Dunbartonshire – Naloxone Project
This initiative is the East Dunbartonshire component of the overall campaign for the National Naloxone Programme of which the overall aim is to contribute to a reduction in fatal opioid overdoses in Scotland.
Naloxone is a medication that temporarily reverses the effects of opioid overdose, available to anyone at risk of opioid overdose.
The service, through our Senior Community Addiction Worker Lorna Deazeley, has provided potentially lifesaving Naloxone training and resources to 140 people in 2021/22. This has made a significant contribution to the harm reduction agenda, in line with MAT standards. Lorna and the service are passionate about helping the people we support and their families.
Volunteer of the Year
The Champions Board
This is a group of Care Experienced Young People who are providing support and influencing statutory agencies and corporate parents on working with Young People.
The Champion’s Board was re-launched in March 2022 following a break during COVID-19. Since the relaunch young people have consistently met on a fortnightly basis. The Champion’s Board currently consists of a core group of 14 young people aged between the ages of 15-25, all with care experience.
The work of the “champs” board is making a significant impact across services in East Dunbartonshire by giving them a better insight into the lived experiences of young people with care experience. This enables services to respond appropriately and increase participation and improve outcomes.
Oral Health Directorate – Leader Of The Year (Joint Winners)
Sharon Hunter
Sharon has demonstrated outstanding leadership qualities, she has promoted positive values and shown respect and dignity during a very challenging time while remobilising our Oral Health Improvement Team.
She has shown continual kindness to staff helping to build confidence and resilience, she has developed a culture of dignity and respect which the staff have responded to in a positive way.
Our wider team have taken this culture on board which has resulted in a more positive environment, helped to inspire others to be more patient and empathic towards each other in a particularly challenging situation.
Karen Lindsay
Karen has been recently appointed interim operational support manager to the Oral Health Improvement Team (OHIT). The OHIT deliver national and local oral health improvement programmes.
During this time as interim support manager, Karen has shown great leadership by supporting the department during the re-mobilisation of oral health improvement programmes, and mentoring 3 new team leads by instilling motivation and encouraging all the team to look after their health and wellbeing
Karen’s influence and positive attitude has allowed the team to implement the new Fluoride Varnish dispensing procedures with a reduction in cost to clinical waste and plastics.
Karen is always looking for ways to make working tasks easier and more efficient e.g. promoting sustainability within our Childsmile programmes.
Oral Health Directorate – Team Of The Year
Oral Health Improvement Team
Oral Health Improvement Team and Public Dental Service worked in partnership to deliver the National Dental Inspection Programme (NDIP).
Prior to the clinical team visiting schools to deliver inspections, the Oral Health Improvement Team (OHIT) visited a total of 317 schools to complete a site survey thereby ensuring that the inspection sites were COVID-19 compliant and discuss any changes or equipment required with Head Teachers.
The Oral Health Improvement Team provided assistance not only with completing site surveys but also on occasion prepared the children for the inspection by acclimatisation visits. 317 schools were visited with an approximately total of 14,490 children having been inspected within the time scale of 4 months.
Oral Health Directorate – Innovation Of The Year
Dental Staff Bank
In late, 2021 as the Public Dental Service (PDS) attempted to remobilise dental services throughout NHSGGC, we identified that General Dental Practices (GDPs) had begun to deregister patients, thus increasing clinical demands on the PDS and necessitating a need to increase the number of staff available to work within Emergency Care Dental Clinics.
Therefore, permission was sought to design and develop a Dental Staff Bank to better manage capacity. A Dental Team lead was appointed to support the recruitment of staff and the allocation of sessions to this innovative scheme.
To ensure compliance with GDC regulations Practitioner Registration, PVG and Occupational Health status was checked as appropriate and staff were allocated session within day time and out of hours clinics.
Specialist Children Services – Innovation of the Year
Physiotherapy input to the National Child Psychiatric Inpatient Unit
The National Child Inpatient Unit, had never had a physiotherapy resource. A test of change was initiated and physiotherapy commenced with individual patients. Some examples include:
- Promoting normalisation of naming body parts and discussing how different parts of the body contribute to movement.
- Education around activity levels, increasing recognition of different types of activity and the balance of energy required to allow our body to work optimally.
- Establishing appropriate low impact, low energy output activity to be able to be carried out within the constraints of weight restoration.
- Exploration of activities to promote relaxation such as yoga and massage.
- Using physical activity to challenge restrictive ritualistic behaviours, and promote positive universal life style changes.
Specialist Children Services – Leader of the Year
Julie Metcalfe
Julie emulates the portrayal of an ideal leader. She is committed passionately to the development of CAMHS services in conjunction with the CAMHS professional leads.
She encourages each individual CAMHS team members, to be the best they can be. Allows individuals / teams to grow, she listens, is solution focused and encourages others to strategically plan and promotes ‘thinking outside the box’. Julie encourages self-wellbeing and a learning culture.
Julie inspires others to work collaboratively and creatively constantly improving and developing the services provided to patients. She promotes a work environment that is respectful, collegial and supportive.
Her Mental Health network spreads far and wide and includes collaborations with the Scottish Government. Julie is an excellent role model and an asset to the NHS.
Specialist Children Services – Team of the Year
GGC: Maternity & Neonatal psychological Intervention service
The GGC Maternity & Neonatal Psychological Interventions (MNPI) service is part of the Scottish Government’s recent commitment to fund perinatal mental health services across Scotland.
The multidisciplinary service addresses the common and/or mild to moderate psychological needs of the maternity and neonatal populations by providing in-patient and out-patient assessments and a range of evidence based psychological interventions.
The central focus in all of these interventions is to enhance the parent-infant relationship, improve parental and infant mental health and to prevent a range of psychological difficulties (emotional and cognitive) in childhood and later life.
The multidisciplinary aspect of MNPI has allowed women to have access to a range of specialist skills so that they receive the best psychological care during their pregnancy and into the postnatal period.