Please use the contact form below to get in touch.
We will do our best to answer any questions as quickly as possible.
Please use the contact form below to get in touch.
We will do our best to answer any questions as quickly as possible.
NHS Scotland participation in the scheme created by The Redress for Survivors (Historical Child Abuse in Care) (Scotland) Act 2021.
On 6 December 2021, Scotland’s NHS Boards were formally invited to participate in the Redress Scheme for survivors of historical child abuse in residential care settings in Scotland.
We acknowledge the wrongfulness of historical child abuse, and the harm this caused to survivors. We offer our full and sincere apologies to anyone who suffered harm and abuse while in the care of NHS Scotland.
We recognise that this Scheme seeks to acknowledge and provide tangible recognition of past harm, and its impact on survivors. Participation in the Redress Scheme is a practical part of our national apology to children who suffered harm while in NHS care.
Further, we recognise that financial redress is only one aspect of acknowledging past harm within care settings for vulnerable children in Scotland.
All 22 of Scotland’s NHS Boards are fully committed to supporting the Redress Scheme. By contributing to the Scheme, we are setting out the commitment from NHS Scotland to support survivors and take steps to provide some redress for past trauma.
We therefore commit to living our values of care and compassion by pledging to be open, transparent and caring in how we engage with anyone who was in the care of NHS Scotland and who makes an application for a redress payment.
Information on the Scheme and support for people affected by this issue can be found through the following links:
This report sets out examples of wider (i.e., in addition to the redress scheme including non-financial) redress activities undertaken by NHS Scotland Health Boards from 7 December 2021 to 7 December 2022 as indicated in the Redress For Survivors (Historical Child Abuse In Care) (Scotland) Act 2021: Statutory Guidance.
Please see the consensus statement on metastatic surveillance of uveal melanoma in Scotland. This gives up to date information on how often we check your body for spread of eye melanoma.
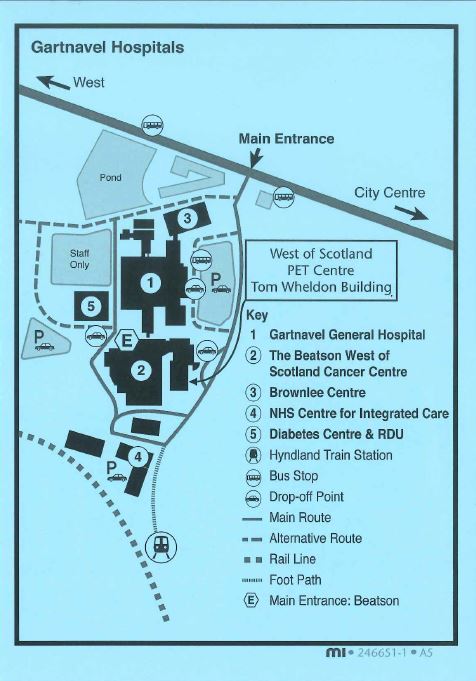
The Molecular Radiotherapy (MRT) service offers a range of radionuclide therapies at Gartnavel General Hospital (GGH) and The Beatson West of Scotland Cancer Centre (BWoSCC) and is staffed by a friendly and professional multi-disciplinary team. The team includes medical doctors, technicians, nurses, physicists, healthcare support workers and clerical staff. Therapies take place in either Beatson main out patients, ward B3 or Nuclear medicine GGH.
Monday to Friday, 8.30am – 4.00pm (Closed Public Holidays & weekends)
If for any reason you are unable to attend your appointment, please inform us by telephoning 0141 301 7621 as soon as possible during office hours to contact your nurse specialist. We will make every effort to adjust your appointment.
Therapies take place across multiple sites on the Gartnavel campus. Please see your patient info leaflet, which will come with your appointment, for location details.
The Beatson West of Scotland PET centre is located on the Gartnavel Hospital Campus. If you have been referred for a PET-CT scan, we will post you an appointment letter, patient information leaflet and directions to the PET Centre. These should provide all the necessary information regarding where and when to attend, what preparation is required and answer many other questions you may have. However, should you have any further queries regarding your PET-CT scan, please call the department on 0141 301 7800 and staff will be happy to help.
Below is a video of what to expect when attending the department for a PET scan. Subtitles can be enabled in the settings menu at the bottom right of the video.
The West of Scotland PET Centre is on the Gartnavel Hospital Campus in the Tom Wheldon building of the Beatson Cancer Centre;
1053 Great Western Road, Glasgow, G12 0YN
The Scottish Ambulance Service has a central booking service which allows you to book ambulance transport. If you require this service, please phone 0300 123 1236 at least 3 days before your appointment but no sooner than 30 days in advance. Lines are open from 8.00am to 8.00pm Monday to Saturday.
There are several options available if you require Hospital Transport Services to attend your appointment. Please see contacts below:
When a baby is identified as a carrier of sickle cell disease it is important to test the parents, if not done before. This way it can be confirmed from which parent this has been inherited and, at the same time, it ensures there are no risks for future pregnancies.
When either parent has been confirmed as a carrier of sickle cell, information on their implications can be found in the following page:
Test baby’s parents, if not done previously (that includes: haemoglobin screen, full blood count and ferritin levels). This can be done in primary care.
If the couple has other children, only test them if the parent is a carrier of any other haemoglobin variant. Otherwise, there is no need to test them unless they are present with health problems. It is normally recommended to postpone testing until the age of 16, to enable them to make their own informed decision.
Stress that other family members can be carriers, so it is advisable to circulate the information to first-degree relatives (parents and siblings) They can request a test called “Haemoglobinopathy screen” via their GP
Make sure the patient understands the rare health issues associated with being a carrier. They should therefore be advised to:
Refer children and adults with haematuria.
Refer children and adults urgently if they present symptoms suggestive of renal medullary cancer. Symptoms include: haematuria, weight loss, loin pain, fever and abdominal pain.
Give the appropriate information leaflets (“Information for mums and dads: your baby carries a gene for sickle cell” and “You are a sickle cell disease”).
Make sure the patient has received his/her haemoglobinopathy card.
Explain that it is still important to have malaria prophylaxis if visiting an area where malaria is endemic.
If you would like more information about haemoglobinopathies and testing, please do not hesitate to contact:
Community Genetic Counsellors on Tel: 0141 354 9201/ 0141 354 9229 (secretary)
When a baby is identified as a carrier of haemoglobin C it is important to test the parents, if not done before. This way it can be confirmed from which parent this has been inherited and, at the same time, it ensure there are no risks for future pregnancies.
When either parent has been confirmed as a carrier of haemoglobin C, information on their implications can be found in the following page:
Test baby’s parents, if not done previously (that includes: haemoglobin screen, full blood count and ferritin levels). This can be done in primary care.
If only one parent is a carrier of haemoglobin C, the couple has a 1 in 2 chance (or 50%) to have children who are healthy carriers.
If the couple has other children, only test them if the partner is a carrier of sickle cell disease. Otherwise, there is no need to test them unless they are present with health problems. It is normally recommended to postpone testing until the age of 16, postpone testing until the age of 16, to enable them to make their own informed decision.
Stress that other family members can be carriers, so it is advisable to circulate the information to first-degree relatives (parents and siblings) They can request a test called “Haemoglobinopathy screen” via their GP.
Give an appropriate information leaflets. (“Information for mums and dads: your baby carries a gene for unusual haemoglobin” and “You are a carrier of haemoglobin C”).
Make sure the patient has received his/her haemoglobinopathy card.
Explain that it is still important to have malaria prophylaxis if visiting an area where malaria is endemic.
If you would like more information about haemoglobinopathies and testing, please do not hesitate to contact:
Community Genetic Counsellors on Tele: 0141 354 9201 / 0141 354 9229 (secretary)
When a baby is identified as a carrier of haemoglobin E it is important to test the parents, if not done before. This way it can be confirmed from which parent this has been inherited and, at the same time, it ensures there are no risks for future pregnancies.
When either parent has been confirmed as a carrier of haemoglobin E, information on their implications can be found in the following page:
Newborn screening: Your baby carries a gene for Haemoglobin D – GOV.UK (www.gov.uk)
There are 7 different types of haemoglobin D. The only clinically relevant variant is haemoglobin DPunjab.
Test partner, if not done previously (that includes haemoglobin screen, full blood count and ferritin levels).
If the couple has children, only test them if the partner is a carrier of a haemoglobin variant. Otherwise, there is no need to test them unless they are present with health problems. It is normally recommended to postpone testing until the age of 16, to enable them to make their own informed decision.
Stress that other family members can be carriers, so it is advisable to circulate the information to first-degree relatives (parents and siblings).
Give the appropriate information leaflets.
Make sure the patient has received his/her Haemoglobinopathy card.
Explain that it is still important to have malaria prophylaxis if visiting an area where malaria is endemic.
If you would like more information about haemoglobinopathies and testing, please do not hesitat to contact:
Community Genetic Counsellors on Tele: 0141 354 9201 / 0141 354 9229 (secretary)
When a baby is identified as a carrier of haemoglobin E it is important to test the parents, if not done before. This way it can be confirmed from which parent this has been inherited and, at the same time, it ensures there are no risks for future pregnancies.
When either parent has been confirmed as a carrier of haemoglobin E, information on their implications can be found in the following page:
If a carrier is found to have reduced MCV and MCH indices, iron supplementation is not required unless the patient’s ferritin levels are reduced.
Test baby’s parents, if not done previously (that includes: haemoglobin screen, full blood count and ferritin levels) This can be done in primary care.
If the couple has other children, only test them if the partner is a carrier of beta thalassaemia or sickle cell disease. Otherwise, there is no need to test them unless they are present with health problems. It is normally recommended to postpone testing until the age of 16, to enable them to make their own informed decision
Stress that other family members can be carriers, so it is advisable to circulate the information to first-degree relatives (parents and siblings). They can request a test called “haemoglobinopathy screen” via their GP.
Give the appropriate information leaflets (“Information for mums and dads: your baby carries a gene for unusual haemoglobin” and “You are a carrier of haemoglobin E”).
Make sure the patient has received his/her haemoglobinopathy card.
Explain that it is still important to have malaria prophylaxis if visiting an area where malaria is endemic.
Community Genetic Counsellors on Telephone: 0141 354 9201 / 0141 354 9229 (secretary)
When a baby is identified as a carrier of haemoglobin Lepore it is important to test the parents, if not done before. This way it can be confirmed from which parent this has been inherited and, at the same time, it ensures there are no risks for future pregnancies.
When either parent has been confirmed as a carrier of haemoglobin Lepore, information on their implications can be found in the following page:
https://www.gov.uk/government/publications/haemoglobin-lepore-carrier-description-in-brief
If a carrier is found to have reduced MCV and MCH indices, iron supplementation is not required unless the patient’s ferritin levels are reduced.
Test the baby’s parents, if not done previously (that includes haemoglobinopathy screen, full blood count and ferritin levels). This can be done in primary care.
If the couple has other children, only test them if the partner is a carrier of beta thalassaemia or sickle cell disease (haemoglobin S). Otherwise, there is no need to test them unless they are present with health problems. It is normally recommended to postpone testing until the age of 16, to enable them to make their own informed decision.
Stress that other family members can be carriers, so it is advisable to circulate the information to first-degree relatives (parents and siblings). They can request a test called “Haemoglobinopathy screen” via their GP.
Give the appropriate information leaflets (“Information for mums and dads: your baby carried a gene of unusual haemoglobin” and “You are a carrier of haemoglobin Lepore”).
Make sure the patient has receive his/her haemoglobinopathy card.
Explain that it is still important to have malaria prophylaxis if visiting an area where malaria is endemic.
Community Genetic Counsellors on Telephone: 0141 354 9201 / 0141 354 9229 (secretary)
When a baby is identified as a carrier of haemoglobin OArab it is important to test the parents, if not done before. This way it can be confirmed from which parent this has been inherited and, at the same time, it ensures there are no risks for future pregnancies.
When either parent has been confirmed as a carrier of haemoglobin OArab, information on their implications can be found in the following page:
If a carrier is found to have reduced MCV and MCH indices, iron supplementation is not required unless the patient’s ferritin levels are reduced.
Test the baby’s parents, if not done previously (that includes: haemoglovinopathy screen, full blood count and ferritin levels). This can be done in primary care.
If the couple has other children, only test them if one parent is a carrier of OArab and the other is a carrier of beta thalassaemia or sickle cell disease (haemoglobin S). Otherwise, there is no need to test them unless they are present with health problems. It is normally recommended to postpone testing until the age of 16, to enable them to make their own informed decision.
Stress that other family members can be carriers, so it is advisable to circulate the information to first-degree relatives (parents and siblings). They can request a test called “Haemoglobinopathy screen” via their GP.
Give the appropriate information leaflets (“Information for mums and dads: your baby carries a gene for unusual haemoglobin” and “You are a carrier of haemoglobin OArab).
Make sure the patient has received his/her haemoglobinopathy card.
Explain that it is still important to have malaria prophylaxis if visiting an area where malaria is endemic.
If you would like more information about haemoglobinopathies and testing, please do not hesitate to contact:
Community Genetic Counsellors on Telephone: 0141 354 9201 / 0141 354 9229 (secretary)
When a patient is identified as a carrier of haemoglobin C, information on their implications can be found in the following leaflet and ordered via PHRD.
It is important to offer testing to the partner to make sure there is no risk to have a baby with a haemoglobin disorder. Ideally, results from both parents’ results should be available before week 12 of pregnancy to enable decisions regarding prenatal diagnosis. Information for fathers on haemologlobin C carrier screening, can be downloaded or ordered via PHRD.
If you would like more information about haemoglobinopathies and testing, please do not hesitate to contact:
Telephone: 0141 354 9201 (receptionist)/0141 354 9229 (secretary)
When a patient is identified as a carrier of haemoglobin D, information on their implications can be found in the following leaflet and ordered via PHRD.
It is important to offer testing to the partner to make sure there is no risk to have a baby with a haemoglobin disorder. Ideally, results from both parents’ results should be available before week 12 of pregnancy to enable decisions regarding prenatal diagnosis. Information for fathers on haemoglobin D carrier screening, can be downloaded or ordered via PHRD.
If you would like more information about haemoglobinopathies and testing, please do not hesitate to contact:
Telephone: 0141 354 9201 (receptionist)/0141 354 9229 (secretary)
What does this mean to the patient?
When a patient is identified as a carrier of haemoglobin E, information on their implications can be found in the following leaflet and ordered via PHRD.
It is important to offer testing to the partner to make sure there is no risk to have a baby with a haemoglobin disorder. Ideally, results from both parents’ results should be available before week 12 of pregnancy to enable decisions regarding prenatal diagnosis. Information for fathers on haemologlobin E carrier screening, can be downloaded or ordered via PHRD.
If patient is found to have reduced MCV and MCH indices, iron supplementation is not required unless the patient’s ferritin levels are reduced.
If you would like more information about haemoglobinopathies and testing, please do not hesitate to contact:
Telephone: 0141 354 9201 (receptionist)/0141 354 9229 (secretary)
When a patient is identified as a carrier of haemoglobin Lepore, information on their implications can be found in the following leaflet and ordered via PHRD.
It is important to offer testing to the partner to make sure there is no risk to have a baby with a haemoglobin disorder. Ideally, results from both parents’ results should be available before week 12 of pregnancy to enable decisions regarding prenatal diagnosis.
Information for fathers on haemoglobin Lepore screening, can be downloaded or ordered via PHRD.
If you would like more information about haemoglobinopathies and testing, please do not hesitate to contact:
Telephone: 0141 354 9201 (receptionist)/0141 354 9229 (secretary)
When a patient is identified as a carrier of haemoglobin OArab, information on their implications can be found in the following leaflet and ordered via PHRD.
It is important to offer testing to the partner to make sure there is no risk to have a baby with a haemoglobin disorder. Ideally, results from both parents’ results should be available before week 12 of pregnancy to enable decisions regarding prenatal diagnosis. Information for fathers on haemologlobin OArab carrier screening, can be downloaded or ordered via PHRD.
If you would like more information about haemoglobinopathies and testing, please do not hesitate to contact:
Telephone: 0141 354 9201 (receptionist)/0141 354 9229 (secretary)
When a patient is identified as a carrier of beta thalassaemia, information on their implications can be found in the following leaflet and ordered via PHRD.
It is important to offer testing to the partner to make sure there is no risk to have a baby with a haemoglobin disorder. Ideally, results from both parents’ results should be available before week 12 of pregnancy to enable decisions regarding prenatal diagnosis. Information for fathers on Beta Thalassaemia carrier screening, can be downloaded or ordered via PHRD.
If you would like more information about haemoglobinopathies and testing, please do not hesitate to contact:
Telephone: 0141 354 9201 (receptionist)/0141 354 9229 (secretary)
A haemoglobinopathy screen cannot differentiate between alpha thalassaemia carriers and iron deficiency. For this reason, it is important to interpret the patient’s results in combination with ferritin levels.
It is important to offer testing to the partner to make sure there is no risk to have a baby with a haemoglobin disorder. Ideally, results from both parents’ results should be available before week 12 of pregnancy to enable decisions regarding prenatal diagnosis.
If you would like more information about haemoglobinopathies and testing, please do not hesitate to contact:
Telephone: 0141 354 9201 (receptionist)/0141 354 9229 (secretary)
A haemoglobinopathy screen cannot differentiate between alpha thalassaemia carriers and iron deficiency. For this reason, it is important to interpret the patient’s results in combination with ferritin levels.
It is important to offer testing to the partner to make sure there is no risk to have a baby with a haemoglobin disorder. Ideally, results from both parents’ results should be available before week 12 of pregnancy to enable decisions regarding prenatal diagnosis.
If you would like more information about haemoglobinopathies and testing, please do not hesitate to contact:
Telephone: 0141 354 9201 (receptionist)/0141 354 9229 (secretary)
When a patient is identified as a carrier of delta beta thalassaemia, information can be found in the following leaflet and ordered via PHRD.
It is important to offer testing to the partner to make sure there is no risk to have a baby with a haemoglobin disorder. Ideally, results from both parents’ results should be available before week 12 of pregnancy to enable decisions regarding prenatal diagnosis. Information for fathers on delta beta thalassaemia carrier screening, can be downloaded or ordered via PHRD.
If you would like more information about haemoglobinopathies and testing, please do not hesitate to contact:
Telephone: 0141 354 9201 (receptionist)/0141 354 9229 (secretary)
When a patient is identified as a carrier of sickle cell, information on their implications can be found in the following leaflet:
It is important to offer testing to the partner to make sure there is no risk to have a baby with a haemoglobin disorder. Ideally, results from both parents’ results should be available before week 12 of pregnancy to enable decisions regarding prenatal diagnosis.
If you would like more information about haemoglobinopathies and testing, please do not hesitate to contact:
Telephone: 0141 354 9201 (receptionist)/0141 354 9229 (secretary)
Haemoglobin is a protein that is carried by red blood cells. Its main function is to pick up oxygen in the lungs and deliver it to the peripheral tissues to maintain the viability of cells. Haemoglobin is made from two similar proteins, usually referred to as subunits, which “stick together”. Both subunits must be present for the haemoglobin to function normally. One of the subunits is called alpha, and the other is beta. Inside each subunit, there is a small iron-containing molecule called heme, to which oxygen is bound. Before birth, the beta protein is not expressed. Instead, a chain called gamma is produced.
Like all proteins, the “instructions” to synthesise haemoglobin are found in DNA (the material that makes up genes). Normally, an individual has four genes that code for the alpha protein, or alpha chain. Two other genes code for the beta chain. The alpha chain and the beta chain are made in precisely equal amounts, despite the differing number of genes. The protein chains join in developing red blood cells, and remain together for the life of the red cell.
The composition of haemoglobin is the same in all people. The genes that code for haemoglobin are identical throughout the world. Occasionally, however, one of the genes has a change or variant. Although the changes that produce abnormal haemoglobins are rare, several hundred haemoglobins variants exist. Most variant haemoglobins function normally, and are only found through specialized research techniques. Some haemoglobin variants, however, do not function normally and can produce clinical disorders, such as sickle cell disease.
Haemoglobin A: This is the designation for the most common haemoglobin variant that exists after birth. Haemoglobin A is a tetramer with two alpha chains and two beta chains (a2b2).
Haemoglobin A2: This is a minor component of haemoglobin found in red cells and consists of two alpha chains and two delta chains (a2d2). Haemoglobin A2 generally comprises less that 3% of the total red cell haemoglobin.
Haemoglobin F: Haemoglobin F is the predominant haemoglobin during foetal development. The molecule is a tetramer of two alpha chains and two gamma chains (a2g2).
Haemoglobin S: This is the predominant variant in people with sickle cell disease. The disease-causing gene change is found in the beta chain. The highest frequency of sickle cell disease is found in tropical regions, particularly sub-Saharan Africa, tribal regions of India and the Middle-East. The carrier frequency ranges between 10% and 25% across equatorial Africa.
Haemoglobin C: Haemoglobin C results from a gene change in beta globin. It can cause sickle cell disease when it is inherited with haemoglobin S. It can also cause haemoglobin C disease when two haemoglobin C variants are inherited. Haemoglobin C is most prevalent in Western Africa, especially in Nigeria and Benin.
Haemoglobin E: This variant results from a gene change in the haemoglobin beta chain. It can cause thalassaemia major or intermedia hen coinherited with beta thalassaemia. Haemoglobin E is extremely common in Southeastern Asia (Thailand, Myanmar, Cambodia, Laos, Vietnam, and India) where its prevalence can reach 30-40%.
Haemoglobin D: There are different types of haemoglobin D variants, but the most vlinically significant is haemoglobin DPunjab (also called DLos Angeles). It results from a gene change in the beta globin chain. It can cause sickle cell disease if coinherited with haemoglobin S. As the name indicated, it is most frequent in the Punjab Area (Northwestern India), where the carrier frequency can be around 2%.
Haemoglobin OArab: This variant results from a gene change in the beta globin chain. It can cause sickle cell disease when it is inherited with haemoglobin S. It is more frequent in North Africa, Middle East and Eastern Europe.
Haemoglobin Lepore: Haemoglobin Lepore is an unusual variant that is th product of the fusion of the beta and delta globin genes. It can cause thalassaemia major/intermedia when a person inherits two copies of haemoglobin Lepore, or when it is inherited with beta thalassaemia. It can also cause sickle cell disease when inherited with haemoglobin S. It occurs most frequently in patients originating from the Mediterranean region.
Sickle cell disease is the name for a group of inherited conditions that affect the red blood cells. The most serious type is called sickle cell anaemia. Sickle cell disease mainly affects people of African, Caribbean, Middle Eastern, Eastern Mediterranean and Asian origin. In the UK, it’s particularly common in people with an African or Caribbean family background. People with sickle cell disease produce unusually shaped red blood cells that can cause problem because they don’t live as long as healthy blood cells and they can become stuck in blood vessels. Sickle cell disease is a serious and lifelong condition, although long-term treatment can help manage many of the problems associated with it.
Sickle cell disease is an inherited blood condition. Babies with sickle cell disease are usually well at birth but may start to develop symptoms from around 4 months of age. The symptoms of SCD are:
Because of the sickling, the patients suffer a chronic haemolytic anaemia and the usual 120 half life of erythrocytes falls to 20 days for patients with sickle disease. The chronic haemolysis results in a rapid production of erythrocytes and a FBC that contains reticulocytes, occasional nucleated erythrocytes, target cells and sickle cells. As the spleen becomes compromised with repeated infarctions, Howell-Jolly bodies are also seen.
Several factors can lead to crises in sickle cell disease: hypoxia, dehydration, vascular stasis, fever, cold and acidosis. Anything that leads to hypoxia will promote sickling. Therefore, patients with respiratory compromise due to infection or chronic respiratory diseases are prone to develop sickle crisis.
There is no single best treatment for all people with SCD. Treatment options are different for each person depending on the symptoms. Treatments can include receiving blood transfusions, maintaining a high fluid intake (drinking 8 to 10 glasses of water each day), receiving intravenous therapy (fluids given into a vein) and medications to help with pain. Nowadays, with the proper treatment, most people affected with SCD live normal long lives.
The different forms of sickle cell disease are:
Severe sickle cell disease: symptoms and management similar to that in sickle cell anaemia.
Beta Thalassaemia is generally caused by point mutations or chromosome 11, following a recessive inheritance pattern (meaning that a mutation in each allele is needed to develop the disease). The symptoms of beta thalassaemia differ greatly from one patient to another, depending mostly on the severity of the mutation. Beta thalassaemia includes:
Alpha globin is made by four genes, two on each strand of chromosome 16. Alpha thalassaemia usually occurs by deletion of some of these four genes. Depending on the total number of alpha genes that a patient has, there are different outcomes:
Alpha globin genes:
4 alpha globin genes: most common scenario, person is not a carrier.
3 alpha globin genes: silent alpha thalassaemia carrier. There is overlap between the red blood cell indices of these individuals and those with 4 gene copies, although the MCV may be slightly lower.
2 alpha globin genes: alpha thalassaemia carrier (also called alpha thalassaemia trait). Individuals who have alpha thalassaemia trait are identified by microcytosis, erythrocytosis, hypochromia and mild anaemia. Individuals with a thalassaemia trait will experience no significant health problems except a possible slight anaemia which cannot be treated with iron, with consequent mild fatigue symptoms.
1 alpha globin gene: the person will be affected with haemoglobin H disease. Haemoglobin H disease is characterized by mild to moderate anaemia, hypochromia and microcytosis. Individuals who have haemoglobin H disease generally have a persistent stable state of anemia, which may be accentuated by increased haemolysis during viral infections and by exposure to oxidant medications, chemicals and foods such as sulfa drugs, benzene, and fava beans (similar to individuals who have G6PD deficiency).
As the red cells mature they lose their ability to withstand oxidant stress and haemoglobin H precipitates, leading to haemolysis. Therapy for individuals who have haemoglobin H disease includes folate, avoidance of oxidant drugs and foods and frequent medical check ups.
No alpha globin genes: the absence of alfa chains causes severe anaemia and leads to hydrops foetalis. This diagnosis is frequently made in the last months of pregnancy when fetal ultrasound indicates a hydropic fetus. The mother frequently exhibits toxemia and can develop severe postpartum hemorrhage. These infants are usually stillborn. There can be other congenital anomalies, though none are pathognomonic for alpha thalassaemia major. If the diagnosis is made early, intrauterine transfusions can be performed.
More uncommonly, alpha thalassaemia can also be caused by point mutations in any of the four alfa globin genes. Some examples of these haemoglobin variants are: Constant-Spring, Icaria, Seal Rock, Pakse, Quong Sze, Sun-Praire and Adana.
Screening information for the transgender community is available via the NHS inform website
NHS GGC Public Health Resources Directory is an easy to use online ordering facility for a range of public health and health improvement resources, available free of charge to clients across Greater Glasgow and Clyde – www.phrd.scot.nhs.uk
Public Health Scotland – Publications – Public Health Scotland