Your health
Across NHSGGC we aim to deliver person-centred care. To do this we need to work with everyone – the person, those who matter to them and the other health care professionals involved in their care.
If the person you work with is supported by friends, family or neighbours in a caring capacity you should refer them to carer support services.
Updates to the Future Care Plan Document (June 2025)
Since 2019 we have been storing information about future care planning on Clinical Portal. The document can be edited by any member of staff to record people’s wishes and preferences. It also gives the opportunity to document clinical management plans, record Power of Attorney details as well as DNACPR discussions. A copy of this document is automatically shared with GPs who can update information on the Key Information Summary (KIS). Primary Care staff can read the latest ECS and KIS directions from Scottish Government here. Staff should check both KIS and the Future Care Plan Summary to ensure they have all information available.
In 2023, we started to use the phrase “Future Care Planning” instead of “Anticipatory Care Planning”. This helped us to emphasis how broad these conversations can be, and all the different topics we can talk about.
As of June 2025, our digital documentation on Clinical Portal now reflects this language. There have also been a few other changes to the documentation we wanted to highlight.
The document is now called the ‘Future Care Plan’ Summary, not the “Anticipatory Care Plan” Summary.
You will still find the document stored under “Care Plans” in the category view, or “Acute Specialities GGC” in the speciality view. The phrase “Anticipatory Care Plan” may still appear in places due to legacy systems, but this should not cause alarm. When creating a new plan you should still go to the “Forms & Pathways Tab” and then click “Add/update Future Care Plan” on the left hand side.
Remember if an old version of the plan exists (i.e. it is still called the Anticipatory Care Plan at the top of the form) please “close” the form, so that the new format can be activated at the next update. You can note that there is an older version on file within the “Special Notes” section of the new document. You don’t need to copy all previous information into the new form, staff should use their own discretion to transfer relevant information.
New options for the Job Role, Area and Trigger drop downs
Care Home and Hospice staff should now select this as their “Job Role” and select the appropriate HSCP they are based in as their “Directorate”. This will help us identify local engagement more easily.
Additional “trigger” options have also been added to the digital document including “Hospital At Home” and “Assessed by HomeFirst Response service” – please use these when necessary.
Please note the PDF version of the form does not include these additional triggers, however it can be noted under “Other”.
Confirmation of Power of Attorney Documentation
Staff should ask to see a copy of any Power of Attorney documentation and record when this happened. Some people may be confused between different legal paperwork (Wills, Types of Power of Attorney, Guardianship Orders, Advance Directives etc) so this helps ensure that everyone knows who has the authority to make decisions for someone.
New question on Treatment Escalation Plans
Treatment Escalation Plans (TEPs) are becoming more common in our Acute sites. If someone has a TEP completed while in hospital this should now be recorded in the Future Care Plan, stating the date, which hospital they were in and the level of escalation suggested.
Recording this information will help us monitor TEP uptake as well as alert community staff to some of the conversations that may have occurred already and which they can build on as they continue to have Future Care Planning discussions.
The PDF version of the Summary has also been updated to reflect the new layout and data that is captured on Clinical Portal.
Within the Board, we believe future care planning is everyone’s responsibility. This is one of the reasons that we have chosen the Clinical Portal system to store future care planning information as it is accessible by Acute, Community and Primary Care as well as Social Work. This means that the majority of health and social care professionals can access and update this information.
We acknowledge that different services will have different conversations based on the roles and remits of the team, however by bringing this information into a central location we can easily share information and help to create person-centred care plans which reflect the wants and needs of people. Therefore our Summary should not be viewed as the responsibility of one individual or service, but rather a dynamic document with many people contributing information.
It is also worth re-iterating that conversations about future care should not just be limited to people at or nearing the end of their life. These conversations can be useful for people at any age and stage of their life and the level of planning required will depend on where someone is in their life journey. We are also encouraging all staff to consider whether someone could benefit from a Frailty Assessment using the Rockwood Clinical Frailty Scale, the results of which can be recorded on the online summary. Early identification and monitoring of frailty is important to help create plans which can slow decline or in some cases reverse frailty. From more information about the Clinical Frailty Scale and other staff training visit the Training Hub.
There is a wealth of resources for the public including webpages which explain many different aspects of future care planning. There are leaflets which can be printed off with further information (these can be found on the Useful Documents and Resources section of the webpages) and also recordings of events covering various topics.
Full details of the approach to Future Care Planning within NHSGGC can be found in the Guidance/Standard Operating Procedure Document. Please note this will be updated to reflect the new terminology in coming months.
You can contact ggc.HomeFirst@nhs.scot with any questions or for further information.
Information for Current Staff
Information for New Staff and Students
If you are new to NHSGGC then we would recommend that you take a look at our training hub. This will help you understand what happens in our Health Board and what role you can play. There may also be specific training for your specific role or area. Check with your line manager or practice development team.
Information for Care Home Staff
Was this helpful?
Are you looking after someone? If so you could be a carer.
There are many reasons why people might need some extra support – they could have a physical or mental illness, they may be frail or have a disability, or they could be struggling with an addiction. They might need physical or emotional support or need practical help to manage day to day tasks.
Carers often provide this type of support to relatives, friends or neighbours even though they are not paid to do so. Carers might not live with the person they support and can be any age.
If you think you might be a carer, you are not alone. There is help and support for you and the person you look after.
Announcement – Changes to the Unpaid Carer Referral Process
As of the 1st May 2024, the Carers Information Line (CIL) will no longer be operational. Whilst a new central referral process is being explored, all unpaid carers can be referred directly to their local services. For contact information and online referral portals please visit the NHSGGC Carers Pages – https://www.nhsggc.scot/your-health/carers/contact-information/
If you are working or visiting an acute site you can visit one of the Support and Information Services based within the hospital who can help you with a referral.
In light of this change, staff are asked to review any information they may have either on webpages, leaflets or in public areas and remove any information which still has the Carers Information Line number (0141 353 6504). These will likely be any yellow posters/flyers that have the title “Are you looking after someone?” or posters/leaflets from Glasgow City HSCP with the same title.
Staff are reminded that everyone has a duty to support carers and signpost them to local support. Local services can provide information, income maximisation, training, emotional support and ensuring carers have a voice in local and political decisions making.
If you have any questions please email ggc.HomeFirst@ggc.scot.nhs.uk
Was this helpful?
Help with these feelings
At times in our life, we can all find it difficult to cope, sometimes we harm ourselves or think of ending our lives.
Self-harm is a way of coping with very deep distress. The ways in which people harm themselves vary and can be physical such as cutting or less obvious such as putting themselves in risky situations or not looking after their physical or emotional needs.
There are many different ways people can intentionally harm themselves. These include:
- Cutting or burning their skin
- Punching or hitting themselves
- Poisoning themselves with tablets or toxic chemicals
- Misusing alcohol or drugs
- Deliberately starving themselves (anorexia nervosa) or binge eating (bulimia nervosa)
- Excessively exercising.
People often try to keep self-harm a secret because of shame or fear of discovery. For example, if they’re cutting themselves, they may cover up their skin and avoid discussing the problem. It’s often up to close family and friends to notice when somebody is self-harming, and to approach the subject with care and understanding.
Self-harm is not about trying to get other people’s attention. Usually, self-harm comes from feeling numb or empty, or wanting some relief. It might be linked to feeling depressed or anxious, low self-esteem, drug and alcohol abuse, relationship problems, bullying or worries about sexuality.
There are many reasons people engage in self-harm. If you are self-harming it may be because:
- You want to feel in control in response to overwhelming feelings inside, low self-esteem or a feeling of powerlessness
- You feel you need to punish yourself because you feel “bad” inside or guilty or ashamed about something
- You feel numb or empty inside and want to feel something “real” or “physical”
- You experience difficult memories or flashbacks of past abuse and harming yourself is a way of bringing yourself back to the present.
Self-harm is not a mental health problem in itself, but it is a behaviour, which is often linked to the experience of mental health problems, whether that is depression, anxiety, personality disorder or trauma.
If you are self-harming, you should see your GP for help. You can also call the Samaritans on 116 123 for support.
Suicide is the act of intentionally ending your life. Many people who have had suicidal thoughts say they were so overwhelmed by negative feelings they felt they had no other option at the time. However, with support and treatment they were able to allow the negative feelings to pass.
There is no single reason why someone may try to take their own life, but certain things can increase the risk. A person may be more likely to have suicidal thoughts if they have a mental health condition, such as depression, bipolar disorder or schizophrenia or if they have experienced abuse or trauma in their past. Misusing alcohol or drugs and having poor job security can also make a person more vulnerable.
More Information
What helps
Many people experience thoughts of suicide or self-harm. You are not alone in feeling like this. People struggle to cope at one point or another and going through a range of emotions during this time is common.
Self Harm
There is no magic solution or quick fix for self-harm, and making changes can take time and involve periods of difficulty. It is common to make some progress and then get back into old behaviours again. If this happens to you, remind yourself that this is all part of the process.
It can help to:
- Work out your patterns of self-harm. Are there certain times of the day or week when you are more likely to self harm? It might help to keep a diary to chart this.
- Learn to recognise triggers – What situations are likely to trigger the urge to self harm?
- Learn to recognise urges – What feelings do you have before you self harm? Whereabouts in your body do you feel them?
- Distract from the urge to self-harm –You will often find that the urge will reach a peak and then pass. Listen to music, do housework, exercise, cook a meal, phone a friend. Relaxation techniques like yoga or meditation can help.
- Build your self-esteem –You might want to seek counselling or support for this or use a self-help book or website.
- Look after your general wellbeing – eat regular healthy meals, ensure you get enough sleep, take regular exercise.
- Reach out for support– If you are self-harming regularly it is important to get help. You can speak to your GP or call a support helpline such as the Samaritans (116123 freephone) or Breathing Space (0800 838 587 freephone)
- Do something creative this can help you to express your feelings. For example, write a song, story or blog, paint or draw.
- Spending time every week doing things that you enjoy, such as seeing friends or going for a walk, is also important. Try to make time to do this, no matter what else is going on.
Suicide
Thoughts of killing yourself can be complex, frightening and confusing. Many people have thoughts of suicide at one point or another. Not all people who die by suicide have mental health problems at the time of death. However, many people who kill themselves do suffer with their mental health, typically to a serious degree.
Sometimes, if a person has been feeling low for a long time, suicide can seem like the only logical way to stop feeling like that. However, feeling actively suicidal is often temporary, even if someone has been feeling low, anxious or struggling to cope for a long period of time. This is why getting the right kind of support at the right time is so important.
If you’re reading this because you have, or have had, thoughts about taking your own life, it’s important you ask someone for help. It’s probably difficult for you to see at this time, but you’re not alone and there is help available.
- Samaritans 116 123
- Breathing Space 0800 838 587 (Freephone)
- If you find yourself in an emergency please call NHS 24 on 111.
Living with thoughts of self-harm or suicide
Thoughts of harming yourself can be deeply distressing. Having these thoughts and urges can make you feel isolated from other people as you don’t want to worry them or burden them with your difficulties. This can make it difficult to be supported by others at the time you need it most. It is important to remember that feeling actively suicidal is often temporary, even if you have been feeling low or struggling to cope for a long time. The urge often reaches a peak and then passes. This is why getting the right kind of support at the right time is so important.
The same applies to living with the urge to harm yourself. Self harm often develops as a way of managing difficult feelings. Once you become dependent on it as a way of managing these feelings, it can be difficult to stop. Again, it is important to remember that the urge often reaches a peak and then passes. Acknowledging that you are struggling and seeking help and advice is an important first step towards recovery.
If you’re reading this because you have, or have had thoughts about taking your own life, it is important you ask someone for help. It’s probably difficult for you to see at this time, but you are not alone and there is help available.
If you find yourself or someone you know in an emergency please call NHS24 on 111
These are free phone numbers, which offer confidential listening, advice and support:
Samaritans 116 123
Breathing Space 0800 838 587 (Freephone)
Looking after someone who has suicidal or self harming thoughts
It can be very upsetting to be close to someone who self-harms – but there are things you can do. The most important is to listen to them without judging them or being critical. This can be very hard if you are upset yourself – and perhaps angry or frightened – about what they are doing. Try to concentrate on them rather than your own feelings – although this can be hard. It is important to remember that most people who self harm do it as a way to cope and live with difficult feelings. It does not mean that they are suicidal. However, self harm should always be taken seriously and it is important not to minimise or dismiss the behaviour.
Things that you can do to help include:
- Let your friend or family member know that you are there, if and when they are ready to talk. It is common for people to worry that they will be judged for their self-harm or that they will be a burden on others, so it’s important to let them know you are there for them if they want.
- Show concern for their injuries, but at the same time, relate to them as a whole person rather than just someone who self-harms.
- Offer them a chance to talk about how they are feeling. Try to understand and empathise with what they are saying even when it is hard to hear.
- Try to understand that they may be scared of stopping self-harm if they use it as a way of coping. If they are finding it hard to stop, try to help them find other ways of coping and to seek help if they need it.
- Let them be in control of decisions about support and any plans to reduce or stop their self-harm.
- Emphasise other parts of their life where they are doing well and the good qualities that they have.
Supporting someone who is self-harming can be a long process with many ups and downs. It’s important to take care of yourself– this will help you to be able to stay involved for longer and avoid becoming unwell yourself.
Supporting and caring for a person who is thinking about suicide, or may have attempted suicide previously can be very stressful and difficult. You may feel alone and scared and not know how best to help the person in your life. There are organisations, which can help you.
One of the best things you can do if you think someone may be feeling suicidal is to encourage them to talk about their feelings and to listen with patience to what they say. Try to understand how they must be feeling and try to engage with any part of them that wishes to live.
If there is immediate danger, make sure they are not left alone and contact NHS 24 (111) for advice
Further information for carers is available on the NHS Greater Glasgow and Clyde carers site
Further information and support
At times in our life we can all find it difficult to cope, sometimes we harm ourselves or think of ending our lives, for help with these feelings please try the following sites.
Self Harm
There is more information about self harm from MIND
The Royal College of Psychiatrists provides a helpful leaflet with information about seeking help for your self harm.
MIND provides information about what family and friends can do to try to help someone who self harms.
If you feel you are drinking too much alcohol or taking illegal drugs these websites may be useful.
There is more information if you are harming yourself through restricted eating or excessive exercise, restricted eating and then bingeing or if you are self harming through intentionally poisoning yourself.
Domestic Violence
- If you are a female experiencing domestic violence here is some information that may be useful for you.
- If you are a male experiencing domestic violence there is some information that may be useful for you.
Personality Disorder
There is information should you feel you may be experiencing a personality disorder.
Survivors of Trauma
For survivors of trauma and abuse these websites may be helpful.
There is information on improving your general self esteem and confidence.
If you have been bereaved or affected by suicide these websites may be helpful.
Self Help Resources
There are self-help guides from Get Self Help, NHS Inform and Help Guide
BSL – Suicide & Self-Harm
NHSGG&C BSL A-Z: Mental Health – Self-Harm
At times in our life we can all find it difficult to cope, sometimes we harm ourselves or think of ending our lives. Self-harm is a way of coping with very deep distress. The ways in which people harm themselves vary and can be physical such as cutting or less obvious such as putting themselves in risky situations or not looking after their physical or emotional needs.
NHSGG&C BSL A-Z: Mental Health – Suicide
Please note that this video is from a range of BSL videos published by NHS Greater Glasgow & Clyde
URGENT HELP
EMERGENCY – If you, or someone you know, need an immediate response call the emergency services on 999.
CONFUSED / DISTRESSED – If you are experiencing confusing or distressing thoughts, or if people around you have expressed concern about your well being, arrange an appointment with your GP or call NHS 24 on 111.
If you, or someone you know, are currently being seen by someone from a community mental health team and require urgent attention, please contact the Out of Hours Team by the number you will have been provided with.
SUPPORT – If you just need to talk with someone, then the following organisations are here to help:
Samaritans – 116 123 (freephone)
Breathing Space – 0800 83 85 87 (freephone)
Please note: if you go to an Accident and Emergency Department because of worries about how you are feeling or what you are experiencing, they will be able to assess your difficulties and arrange for you to see a specialist if needed. But Accident & Emergency is a busy and stressful place, and you may have to wait a long time. It can be quicker to phone NHS 24 on 111, as they can arrange for you to get to the right help.
Heads Up is not continuously monitored and is not able to provide direct advice or support to those in mental health distress.
Was this helpful?
Stress is the experience of the feeling that the demands upon us are greater than our resources to cope. People can cope with many difficult tasks but when an extra task is added they feel stressed, one extra demand on someone’s resources can push them into feeling stressed, as described by the phrase ‘it was the straw that broke the camel’s back’.
Stress can be an overwhelming experience and can be understood as pressure from others or being put in situations that you find difficult to cope with. It can also occur when you feel that you don’t have much control over a situation.
More Information
Where does stress come from? The Flight or Fight Response…
The ‘Flight or Fight’ response
The ‘fight or flight response’ is our body’s own protective response to danger and, in essence, it is a mechanism designed to protect us, and not as it feels, destroy us.
Our bodies are designed to respond to danger; we have an inbuilt defence mechanism known as the ‘fight or flight response’, which triggers psychological and physical changes in our bodies. The release of chemicals can give very real physical symptoms such as rapid heart rate and breathing. These symptoms are designed to give us the ability to ‘fight or flee’ a specific danger, however for a panic attack sufferer, someone who suffers from anxiety or someone experiencing stress, these feelings can feel intensified and with no present danger.
Why do we have the “Flight or Fight” response?
This sudden burst of adrenaline, the increased oxygen and heart rate, gives our bodies increased abilities and sensory perception – which if you need to flee a wild beast or save your family from a burning building will indeed be used to maximum effect. If however you are simply doing your grocery shopping, taking your child to school, or sat watching TV for example, these frightening feelings can be extremely difficult to cope with or explain.
If there is no need to use the excess chemicals; adrenaline or the increased oxygen supply, then our bodies begin to act against us, the decreased carbon dioxide levels in our lungs and blood causes us to feel dizzy and disoriented, we can begin to hyperventilate and a panic attack can ensue.
What can I do to help if I feel stressed?
There are a range of things you can do if you feel like you are stressed regularly. There are physical activities and mental tricks you can try to help; some are activities you can implement when you are in a stressful moment and others are things you can do to try and reduce your overall stress levels and prepare for future challenging times.
- Be Active
- Take Control
- Connect with people
- Have some me time
- Challenge yourself
- Avoid unhealthy habits
- Work smarter not harder
- Be positive.
Living with stress – how does stress feel?
Stress is frequently described as the feeling of being under pressure. Some people describe feeling under threat, anxious, tense, tearful or agitated. Often these feelings are accompanied by physical sensations. It is important to note that these reactions are normal but everyone experiences stress in their own way so your reaction may appear to be different from a friend or family member’s.
If stressful times pass, the body will usually return to normal functioning after a period of time. However if you feel that you have been stressed for some time you make be advised to seek support from your GP.
Looking after someone with…stress – how might we notice if someone is stressed?
When people are stressed they can make choices they would not usually make and behave in a way that is a little different from usual. From the outside you might notice a person saying or doing things that are out of character, someone struggling to concentrate, physically appearing more tired than usual, eating and drinking more or less than usual, taking more or less time over their general presentation than usual and/or appearing to be rushing or forgetful.
Stress is something many people feel for short periods in life but difficulties arise if this experience persists.
Further information for carers is available on the NHS Greater Glasgow and Clyde carers site
How can I support someone else who seems stressed?
Whilst the above resources will be helpful for your understanding of stress, the award-winning Power of OK campaign from Scotland’s See Me programme gives some very practical advice and contains an accessible video resource to explain all (videos contains strong language)
Further information and support
One resource you may find helpful for coping with stress is the Glasgow Wellbeing resource, which includes a free guide to download, and relaxation videos. In addition, the website has a range of other support materials to help you think about the causes of stress.
Glasgow Wellbeing is full of helpful and informative resources
NHS Choices suggest 10 tips to beat your stress.
This is an NHS resource with instructions for breathing exercises, which are recommended to help ease the feeling of stress
Resources created specifically for young people
The Royston Stress Centre which offers an outreach service to 11–18 year olds in North Glasgow have made an excellent film to help young people understand stress:
Ayemind website contains child-friendly resources explaining stress and includes information on child-specific stressors such as school exam stress
The Royal College of Psychiatrists have a leaflet for young people who are managing stress
A free mobile application called SAM – Self Help for Anxiety Management – has some useful resources and can be carried around with you subtly on your phone
SafeSpot is a brand new app for iPhone and Android that promotes positive mental wellbeing in children and young adults.
If you need someone to talk to
Breathing Space Scotland has a phone line and an associated therapy service called Living Life
Samaritans offer a 24/7 confidential support service which includes a phone line: 0141 248 4488, a freephone number: 116 123 and an email service: jo@samaritans.org
BSL – Stress
NHSGG&C BSL A-Z: Mental Health – Stress
Stress is normal and it affects everyone. It usually happens when you are in a situation that puts you under pressure. It can happen when you have lots to think about or do or when you don’t feel you have much control over a situation. It usually happens when you have things to do that you find difficult to cope with. Many situations can cause stress including relationships, work demands, financial worries and so on. It can have an effect on our emotions, thoughts, behaviour and physical wellbeing
Please note that this video is from a range of BSL videos published by NHS Greater Glasgow & Clyde
Was this helpful?
What is low self-esteem?
Self-esteem is a term used to describe how you view or think about yourself and the value that you place on yourself.
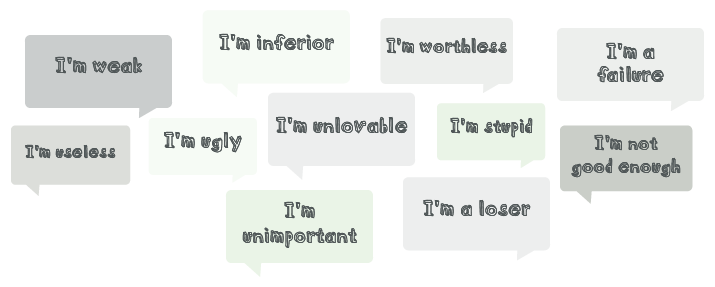
When faced with stressful or challenging situations, it’s common for people to use negative words to describe themselves, such as ‘I’m useless’, ‘worthless’ and ‘not good enough’. However, if you often think about yourself in these terms, then you may be experiencing low self-esteem. Someone with low self-esteem may have a generally negative opinion of themselves. Common thoughts that someone with low self-esteem may have are:
Do you have low self-esteem?
There are self esteem test that can be completed online or downloaded as a paper version
More Information
How does low self-esteem develop?
Often, beliefs about ourselves are conclusions we arrive at due to the things that have happened to us in our lives. If you’ve encountered negative experiences in your life, particularly in your childhood, you may hold very negative thoughts and beliefs about yourself.
If you have been neglected, mistreated, abandoned, abused or punished in extreme or unpredictable ways, you can come to believe very negative things about yourself and these experiences may cause you to develop low self-esteem.
Constantly being criticised can also cause you to develop negative beliefs about yourself. Your parents, carers or other family members making fun of you or highlighting your weaknesses instead of acknowledging your successes and strengths can also have a negative impact on your self-esteem.
Other factors that cause low self-esteem are:
- Feeling as if you do not fit in anywhere (at home, at school)
- Feeling intellectually inferior to or less talented than your siblings or peers
- Feeling that you or your family is considered different or less socially acceptable by others
- If your family was on the receiving end of prejudice or hostility
- If you had an emotionally distant parent or carer
- If you had a parent or carer who was not physically affectionate or able to spend time with you
- If you did not receive enough attention, encouragement, warmth or praise as a child.
If your parents had to give their attention to dealing with stressful or difficult life events and were therefore unable to give you much attention.
What causes low self-esteem…
In young people?
In late childhood and adolescence, physical appearance and how you feel about your body may start to become very important. People around the same age can also influence how you see yourself. If the people around you say negative things about you or tease you about your physical appearance, you may start to feel you are ‘unlikeable’ or ‘ugly’. This is often made worse by messages conveyed by the media, for example, that we should be slim and physically attractive to be worthwhile.
Later in life?
Negative beliefs tend to develop in childhood. However, being bullied or intimidated at work, being in an abusive relationship, experiencing prolonged financial hardship, continuous stressful life events, traumatic events, or life-changing illnesses or injuries can trigger low self-esteem later in life.
What helps
What helps overcome low self-esteem?
Low self-esteem is underpinned by negative thoughts relating to how you view yourself and how you believe others view you. One of the main ways of dealing with low self-esteem is to try and work on these thoughts.
Ways to work on your thoughts
One way of overcoming low self-esteem is to appreciate yourself more and notice your own personal qualities, everyday. Record all the good things about yourself and ask others in your life for help.
At the end of each day, think about what you have done and what personal qualities you displayed. For example, if you went to work that day and arrived on time, the quality you showed was good time management. If you listened to a friend’s worries, then you display qualities such as kindness, empathy, being a supportive friend and a good listener, as well as many more.
The key is to continuously develop a record reflecting your worth so that you can look at this when the negative thoughts creep in.
When the negative thoughts about yourself creep in, challenge them, put them to the test, are they as true as you believe, would they stand up to scrutiny in court. Put your thought (not you) in the dock. Pretend that you are a lawyer paid lots of money to prove to a jury that the thought is true. What would you say? Remember the judge is watching. The judge will only allow evidence to be presented in court, not your opinion. Evidence from expert witnesses can be given, so who would you call to the stand? Next pretend you are the other lawyer, being paid lots of money to prove that the thought is not true and to contradict your fellow lawyer’s evidence. What would you say, what expert would you put on the stand?
You are now a jury member, you’ve heard what the lawyers and their expert witnesses have to say, what will you conclude?
There is more information on this technique and information about facts versus opinions.
Living with Low Self Esteem
Ways to work on your thoughts about your appearance
We are constantly being told if you want to be happy you need to look a particular way or fit a particular style of clothing. Try and see this for what it is, marketing to sell a product. You will never fit into clothes in all shops or match the ideal image that they are portraying because the shops on your high street originate from many different countries where the ideal image and body shape differs greatly.
Ways to work on your behaviour
Try to be assertive and project confidence as this will encourage others to treat you with more respect, which in turn will help you feel more confident and of greater worth. Even if you do not feel confident, you can “fake it until you make it” with some simple behavioural strategies to give the allure of confidence. The Centre for Clinical Interventions has information on the skills in assertiveness that everyone can do no matter how they feel inside.
People with low self-esteem tend to withdraw from the world in general. You may tend to do less of the things you find pleasurable. One way to improve your self-esteem and sense of achievement is to start doing things again a little at a time. Try to make a list of the things you did previously but stopped or new things you would like to do. Use this weekly planner to start reintroducing these activities.
Engaging in physical activities is a great way to build confidence. In fact, a recent study found that women aged 18 to 24 are twice as likely to be confident and have high self-esteem if they play sport. You can get a sense of achievement from physical activity. Due to the chemicals released during exercise, you can also experience an improvement in your mood. If you prefer to exercise alone, you may benefit from downloading an exercise app, such as Runkeeper or Nike+ Training club – workout & fitness plans. These allow you to track your achievements. You can also join the social media forums available so you can get encouragement from others.
Looking after someone with…Low Self-Esteem
How to support someone with low self-esteem
There are several ways to support people with low self-esteem. You can help by continuously pointing out their positive qualities and achievements. You can encourage them to write these compliments down as a record of their own personal qualities.
There are several ways to support people with poor body image. You can point out what their body enables them to do rather than what their body looks like and highlight that everybody looks different.
Advice for parents trying to nurture self-esteem in their children:
As a parent you will be aware that young children are being bombarded with messages about how they should look and behave. Disney characters are often female and beautiful or male and strong. In teenagers there is often talk of the amount of muscles a boy has.
It is important to let our children know that everyone matures at a different rate and everyone has a different body shape, that your looks do not determine your value but rather it is what you achieve and contribute in life and the person that you are that counts.
- Here is more advice for parents on nurturing positive self-esteem
- Here is more advice for parents on nurturing positive body image
- Here is more advice specific to nurturing girls self-esteem from The Amighty Girl.
The Amighty Girl Facebook page is also helpful, as each day information about inspirational girls and women is posted and not one is inspirational because of their looks but rather because they are different and have achieved something great.
Further information for carers is available on the NHS Greater Glasgow and Clyde carers site
Further information and support
If you would like to find out more about self-esteem and ways to improve low self-esteem either in yourself or others, there are several websites listed below that may be helpful.
- Centre for Clinical Interventions
- MIND
- NHS choices
- Kidshealth.org
- Overcoming self-esteem
- Overcoming low self esteem by Melanie Fennell is a self help book and is available online for free and is held by many Glasgow libraries
Was this helpful?
Psychosis can happen to anyone and affects up to 3 in 100 young people in Scotland. Up to 10 per cent of people will at some point in their life hear a voice talking to them when there is no-one there. Many people who have these kinds of experiences do not come into contact with mental health services because they do not find their experiences distressing. Some people, however, are very distressed and find it difficult to cope so they seek professional help, or others seek help on their behalf.
People who seek help with psychotic experiences are sometimes given a diagnosis of schizophrenia or bipolar disorder. Psychosis can also be linked to very severe depression. There are a number of things which seem to be linked to psychosis or to make the symptoms worse. These include:
- Alcohol and drugs, especially street drugs like cannabis, speed (amphetamines) and cocaine. New synthetic drugs (so-called “legal highs”) can cause severe psychotic symptoms
- Other health problems, like head injury or epilepsy
- Severe, prolonged stress or trauma
- Severe social problems such as poverty, isolation or lots of stressors such as poor housing, overwork or relationship difficulties.
It is not clear what causes psychosis but it is probably a complex interaction between life circumstances, the way we see the world and our biological make-up.
There is sometimes confusion about what psychosis means. Psychosis has nothing to do with the terms “psycho”, or “psychopath”. It is very rare for people with a diagnosis of psychosis to be violent to others.
Many people have had one or two brief “psychotic” experiences, and they are not always a cause for concern. But it’s important to speak to your GP about this because some kinds of psychosis need treatment.
Getting help early helps people to make a better recovery.
People with psychosis can’t always recognise what’s happening to them: they might think there’s nothing wrong, and be reluctant to visit their GP. It’s important that family and friends try to persuade them to get help. If that’s not possible, you should consider getting confidential advice from their GP.
More information about psychosis is available from See Me and NHS Choices.
Acknowledgement:
Understanding Psychosis and Schizophrenia (2017) © British Psychological Society licensed under Creative Commons (CC BY-NC-ND)
More Information
What helps
You should see your GP straight away if you are having psychotic experiences. Early treatment of psychosis gives the best chance of recovery.
NHS Choices has some useful information about the kinds of question your GP may ask about psychosis. If they think your psychotic experiences might be caused by mental illness, they will arrange for you to be seen promptly by a specialist.
For people who live in the NHS Greater Glasgow and Clyde area, that is likely to be the “Esteem” team, a service for people with a first episode of psychosis. The team has bases throughout the Greater Glasgow and Clyde area.
Other people may be seen by a Community Mental Health Team (CMHT) in their local area. CMHTs can offer help from the following healthcare professionals:
- A psychiatrist – a qualified medical doctor who has received further training in treating mental health conditions
- A psychologist – a healthcare professional who specialises in the treatment of mental health conditions through talking therapies
- A community mental health nurse – a nurse with specialist training in mental health conditions
The main treatments for psychosis include:
- Medicines – Most people find that antipsychotic medicines (such as risperidone, olanzapine and clozapine) are very helpful. They can reduce or stop hallucinations and help people to think clearly again. They usually take a week or more to start working, and many people take them long-term. However they do have side effects, and it may take some time to find the right drug for you.
- Psychological treatment Cognitive Behavioural Therapy (CBT) for psychosis can be an effective way to tackle unhelpful thoughts and feelings that might be caused by psychosis.
- Family support Behavioural Family Therapy (BFT) is a useful way to help you and your family cope with psychosis, while minimising the stress of living with that condition. It should be available in your area if you live in Greater Glasgow and Clyde.
- Peer support – It’s often helpful to link up with others who have had a similar experience of illness to you. Support in Mind Scotland have particular experience of psychosis. You might also contact the Mental Health Network if you live in Glasgow, or Acumen if you live in Renfrewshire, East Renfrewshire, West Dunbartonshire or Inverclyde.
Find out more about treatments at NHS Choices.
Some people become so ill with psychosis that they’re temporarily unable to make good decisions about their care. If that happens, and there’s a risk to the health and safety of that person or to others, then doctors can use the Mental Health Act in Scotland to ensure people have the right care and treatment. Long-term decisions about care and treatment are made by the Mental Health Tribunal for Scotland, and the Mental Welfare Commission for Scotland works to ensure that peoples’ rights are respected.
Living with…Psychosis
Many people who hear voices or see visions are not troubled by them and do not seek help. For those who do, around half will completely recover after just one occasion. Some people do experience on-going difficulties. When we feel stressed or anxious, the way we think about ourselves, other people and the world around us can change. For example, we may become more self critical or fearful. There are close links between emotional distress and psychosis. Anything we can do to help with emotional problems is therefore also likely to help with symptoms of psychosis. Below are some ideas about ways to manage difficult emotions and stress.
Looking After Yourself
Taking time to look after yourself is an important part of recovery.
Think about:
- Eating regularly
- Getting enough sleep
- Getting some exercise. Exercise is good for mental health as well as physical health. Try to get 30 minutes a day of moderate exercise if you can. NHS Choices has some good suggestions to get started if you’re not used to exercising
- Some people find mindfulness or yoga especially helpful. Although not always available through the NHS, there should be classes in your area
- Keeping in touch with people who make you feel good about yourself
- Avoiding too much alcohol or caffeine, including energy drinks
- Avoiding non-prescription drugs. Cannabis, speed (amphetamines), ecstasy, cocaine, mushrooms and so-called “legal highs” can all make your symptoms worse.
Find a Routine
Everyone needs a reason to get up in the morning so set your alarm. Plan one activity you enjoy and one which gives you satisfaction every day. Try to stick to your plan even if you don’t feel like it at times.
Write down all the things you like doing and people you like to see, and come up with a plan to start doing things and seeing people at your own pace.
If you build up to things at your own pace, over time you’ll be able to do more and more. Your family, friends or your mental health worker can help you make a plan for this.
It may be helpful to keep a diary, recording life events, your mood, your diet and sleep. This can help you recognise patterns in your moods and psychosis, and identify what might trigger it or make it worse. It can also help you identify things that have been helpful, and recognise warning signs that tell you when you are starting to feel worse.
Getting appropriate help
Stay in touch. Make sure that trusted family and friends know how you’re really feeling. It’s important to discuss symptoms, side effects and any other concerns with the clinicians working with you.
Watch out for low mood. Many people experience low mood or depression, either as part of their psychosis or as they recover from psychosis and get back to their usual lives. Let your psychologist, doctor or nurse know about this – they should be able to help. Suicidal thoughts at times are also common, and it’s especially important that you let someone know if that is troubling you.
Since some medicines taken to control psychosis can make you gain weight, it’s really important to know your weight (and BMI), and to eat healthily. Since medicines and weight gain might increase your risk of diabetes or high cholesterol, make sure these are checked by your doctor.
If you are a smoker, do all you can to quit. Stopping smoking will improve your mental health as well as your physical health. The Smokeline service might be able to help.
Managing Symptoms
There are lots of helpful things you can do to help you deal with distressing symptoms. Everyone’s experiences of psychosis are different so not all of these ideas may be useful to you. You could try out some of these ideas as other people have found them helpful.
Hearing Voices
Distraction
Some people are able to get control over their voices by distracting themselves by:
- Humming
- Listening to music
- Talking to or contacting a friend
- Playing computer games or using your phone
- Doing everyday things around the house
- Seeing friends.
Responding to Voices
- Sometimes if you talk to the voices, they will go away. You can talk into your phone when speaking to the voices to avoid bringing attention to yourself
- Imagine turning down the volume on the voices, like you would on the TV
- Keep a note of when the voices speak to you and what they say to see if these things are important to you.
Upsetting Ideas or Beliefs
Keep calm
Even though you may think or feel something is real, it may not be. Very often things we believe strongly can turn out to be wrong, so try to remind yourself of this. Try to work out what is different about times when the belief does not feel so strong and write down what you notice.
Keep busy
When you’re busy playing a sport, doing a bit of work, doing the shopping or hanging out with friends, the ideas can feel less upsetting or important.
Keep safe
Try not to act on your beliefs even if you have a very strong urge to, as this can keep your worries going. Talk to someone you trust – a family member, a friend, mental health worker or psychologist. Be aware that simple things like crossing the road can become difficult when you are very distracted.
Looking after someone with…Psychotic symptoms
As a friend, family member or partner, you can have an important role in supporting your loved one. You can help them learn to manage their psychosis and reduce the likelihood of them becoming unwell.
However, it can be difficult to know how best to help. Below are some suggestions that might be useful to you.
Helping with Unusual Experiences
Hearing voices is often very distressing for someone, as the voices are often critical and say unpleasant things. Some people may wish to talk about what the voices are saying, while others prefer to keep this private.
If the person wishes to speak about their voices, try to understand how they feel, even if you may not agree with their explanation of the voices. You can also try to point out the person’s good points to boost their confidence, as the voices will often try to undermine this.
It can help to distract the person by starting conversations or getting them involved in day-to-day activities. You could also ask the person what works for them as they may have found other ways to cope with the voices.
When people have unusual ideas or beliefs, it can be difficult to understand where these come from. It is often tempting to try to talk them out of their beliefs but this can sometimes lead to heated conversations.
Try to keep calm, even if the person is saying things that seem very frightening, and reassure them by showing them you understand how significant their beliefs are to them.
Helping with Problems with Motivation
Psychosis can make it hard for a person to:
- Think straight
- Keep going
- Take an interest in people
- Keep up with things they previously enjoyed.
While this can be frustrating for those trying supporting them, try not to expect the person to do too much too soon. It is important to strike the balance between gentle encouragement and making allowances for their difficulties. Offer praise for any achievement, however small, and try to find enjoyable or practical things to do together.
What Else Can Help?
Help the person to regain their confidence by encouraging them to do things on their own.
As it can be hard for the person to realise that others in the family may also need support or help, give clear, calm messages about what you would like to happen.
Stick to an everyday routine with regular mealtimes and chores.
Like everyone, the person may need their own time and space, so try to respect this without worrying too much.
As the person can sometimes seem distant or unemotional, show support and acceptance by continuing to spend time with them and involving them in everyday things.
Getting help
Someone who is experiencing a psychotic episode might not be aware of the changes in their thinking and behaviour. It might often fall to friends or family member to support individuals in accessing help. If someone you know needs help urgently, you have two options:
- Make an urgent appointment with their GP
- Call NHS 24 by dialling 111
How services can help family and friends to support people
Many families find it helpful to meet with a professional who is trained in helping families. The aims of these meetings could include: developing a shared understanding of what is happening, improving family relationships, and finding ways to solve problems together. Guidelines recommend that everyone diagnosed with psychosis can access family interventions. These should be available in your area if you live in Greater Glasgow and Clyde.
Even if the person does not want personal information shared with relatives, services can give you general information about the problems people experience, what can help, and what support is available.
While it is important for staff to keep information about the person’s care private, sometimes the people who live with the person or know them well may have ideas or information, which can help in their care. It is fine to pass this information on to staff if you think it might help.
Look After Yourself
Seeing someone you care about experiencing psychosis can be distressing and confusing. It is important to take care of yourself.
It can be difficult to support your relative and look after yourself at the same time. However, it is very important to make time for yourself to ensure that you do not become overwhelmed by what is happening to the person you care about.
This might mean taking time out for yourself and doing the things that are important to you, like seeing friends or keeping up with your interests. Keeping to the same routines in your day-to-day life can also reduce tension at home.
You may also find speaking to others in a similar situation useful.
Below are some resources you may find helpful:
- Support in Mind
- GAMH Carers Support
- Carers Link East Dunbartonshire
- Carers of West Dunbartonshire
- East Renfrewshire Carers Centre
- Renfrewshire Carers Centre
- Inverclyde Carers Centre
Further information for carers is available on the NHS Greater Glasgow and Clyde carers site
Early Intervention
Early treatment of a psychosis gives the best chance of recovery.
An early intervention programme, of up to 2 years, is recommended for people aged 16-35 who appear to be experiencing a first episode of psychosis.
Early interventions, for people who experience a first episode psychosis, are known to positively impact on engagement with mental health services, access to family & other psychological interventions and on future education & employment prospects and social & functional recovery.
Early intervention programmes offer different types of support that have been shown to help people recover from psychosis, and usually include practical support, family work, psychological therapy and medication. There would also be a focus on minimalising the effect of psychosis such as feelings of loss, entrapment and humiliation.
What are the potential long-term problems of untreated psychosis?
The risks include suicide, more likely to relapse, greater resistance to treatment, higher incidence of requiring compulsory care, poorer engagement with treatment, higher rates of substance miss-use, and greater distress amongst family members
“The course of schizophrenia is most stormy at onset and early in its manifest course, plateauing thereafter”
The plateau effect and the critical phase (Birchwood et al, 1998)
What could you expect from an early intervention programme?
There would commonly be a range of support/interventions available, nurses or occupational therapists would help you think about what might be most useful to you, psychiatrists would talk to you about medication options, a clinical psychologist can help with talking therapy, whilst a support worker could help you to get you out and about more.
What about hospital?
Early interventions may sometimes require a short stay in hospital, especially if you are very distressed by their experiences. There could also be some crisis or assertive outreach interventions.
What can early intervention work help with?
Early intervention work will focus on:
- Helping you try to understand the things that led to your experiences of psychosis
- Exploring ways to help with your recovery
- Working with your family and friends to encourage positive relationships
- Offering practical support with things like housing or finances
- Supporting you to return to work, university or college, or identifying ways to spend your time
Early interventions also means working with your family and friends by:
- Involving them in all aspects of your care, if you feel this would be helpful
- Offering group sessions for support
- Offering family work
- Offering individual therapy to family members
What happens after such early intervention?
Early intervention results in many people making a full recovery within two years and do not need follow-up from another mental health service, with their care being returned to their GP.
For others, the recovery process takes longer than two years, and their care is transferred to a local community-based Mental Health Team for further support.
“My memories from the first month of this episode are fairly hazy”
Early Intervention in First Episode Psychosis: A Service User’s Experience
Stephanie Allan; Early Intervention in First Episode Psychosis: A Service User’s Experience, Schizophrenia Bulletin, Volume 43, Issue 2, 1 March 2017, Pages 234–235, https://doi.org/10.1093/schbul/sbv227
Video on Psychosis and how early intervention can help… courtesy of EPUT – Essex Partnership University NHS Foundation Trust
Further information and support
Be informed! These sites can help you learn more about…
What is psychosis?
Maudsley NHS video What is psychosis?
Help for psychosis
The British Psychological Society has written a report called ‘Understanding Psychosis and Schizophrenia’. It has lots of information about what it means to have psychosis and what can help. It has personal stories written by people who have experienced psychosis about what this has been like for them and what has helped.
You can read it here.
Medicines and their side effects
There are published guidelines about the standard of care it is reasonable to expect:
Local and national organisations
- Scottish Recovery Network
- Support in Mind Scotland
- Glasgow Association for Mental Health
- Breathing Space is an NHS helpline that offers emotional support for people experiencing low mood, depression or anxiety. They can be contacted on 0800 83 85 87. They are open Monday to Thursday between 6pm and 2am and Saturday and Sunday between 6pm and 6am.
- See Me Scotland can help you find out more about the stigma of mental illness, and what you can do to stop it in Scotland.
- The Mental Health Act in Scotland, Advance Statements, and your legal rights.
BSL – Psychosis
NHSGG&C BSL A-Z: Mental Health – Psychosis
Psychosis is a term used to describe a number of unusual experiences:
- hearing or seeing things that other people can’t hear or see (hallucinations)
- holding unusual beliefs that people from a similar background would think strange or irrational (this includes delusions and paranoia)
- being so jumbled in thoughts or speech that other people can’t easily make sense of what you are meaning (thought disorder)
- experiencing periods of confusion – for example: becoming very distracted and finding it difficult to pay attention or make decisions
Psychosis can happen to anyone, up to 10 per cent of people will at some point in their life hear a voice talking to them when there is no-one there. Lots of things can contribute to a person experiencing psychosis such as stress, physical illnesses, using drugs or alcohol and mental illnesses
NHSGG&C BSL A-Z: Mental Health – Schizophrenia
Schizophrenia is a serious mental illness that affects thinking, emotions and behaviour. It is the most common form of psychosis. Schizophrenia usually affects people for the first time when they reach early adulthood – from their late teens to early thirties. Symptoms include:
- Hallucinations – hearing, smelling, feeling or seeing something that isn’t there.
- Delusions – believing something completely even though others find your ideas strange and can’t work out how you’ve come to believe them.
- Difficulty thinking – you find it hard to concentrate and tend to drift from one idea to another. Other people can find it hard to understand you.
- Feeling controlled – you may feel that your thoughts are vanishing, or that they are not your own, or that your body is being taken over and controlled by someone else.
Other symptoms include:
- Loss of interest, energy and emotions.
- Problems with motivation and organising yourself.
Problems with routine jobs like washing, tidying, or looking after yourself
Please note that this video is from a range of BSL videos published by NHS Greater Glasgow & Clyde
BSL – Anti-Psychotic Medication
NHSGG&C BSL A-Z: Mental Health – Anti-Psychotic Medication
Anti-Psychotic Medications are an important part of treatment for psychosis. They may need to be taken for a long time to keep well. There are different types of anti-psychotic medication and they can be taken as tablets, injections or as a liquid
Please note that this video is from a range of BSL videos published by NHS Greater Glasgow & Clyde
Was this helpful?
Many of us will experience a traumatic event at some point in our lives. A traumatic event is one where you are in danger, your life is threatened, or where you see other people dying or being injured. Examples of traumatic events include road traffic accidents, assaults and sexual assaults, being involved in a natural disaster such as an earthquake, witnessing or experiencing war, torture or being held hostage.
It is usual for a traumatic event to cause upset and distress. Most people will recover with the support and care offered by family and friends and by using the ways of coping that they would normally use to deal with stress. However, some people will experience distress that is more intense and longer lasting and may result in Post Traumatic Stress Disorder (PTSD)
The main symptoms of PTSD are:
- Re-experiencing – This is when a person involuntarily and vividly re-lives the traumatic event in the form of flashbacks, nightmares, repetitive and distressing images or sensations or physical sensations – such as pain, sweating, nausea or trembling
- Hyperarousal – This means feeling on edge and always on the lookout for danger. This can cause increased anxiety, panic attacks, irritability, anger, sleeping problems and difficulty concentrating.
- Avoidance – This means avoiding reminders of the traumatic event such as places, people, media reports or avoiding talking to anyone about the traumatic experience.
Many people with PTSD try to push memories of the event out of their mind, often distracting themselves with work or hobbies.
Some people attempt to deal with their feelings by trying not to feel anything at all. This is known as emotional numbing. This can lead to isolation and withdrawal and in giving up previously enjoyed activities.
- Negative changes in mood and thoughts – PTSD can also lead to changes in thoughts and feelings. For example many people become preoccupied with trying to understand why the traumatic event occurred and play it over in their minds looking for an answer. This can cause guilt or shame that it happened to them or that they could somehow have prevented it. It can also shake beliefs about the world being a safe place to live.
Other reactions following a trauma include depression (or a worsening of previous depression) and dissociation. Dissociation occurs when a person feels cut off from sensory experience. They may experience short gaps in their memory or periods of depersonalisation or derealisation (feeling on the outside of things, disconnected, as if things aren’t real).
More Information
Complex Post Traumatic Stress Disorder
Complex Post Traumatic Stress Disorder (PTSD) is a term used to describe the changes that people experience following multiple or repeated traumatic events. Examples include childhood sexual, physical or emotional abuse, domestic violence, being held hostage and victims of torture or trafficking. These experiences are interpersonal (caused by a person deliberately harming another person) and become anticipated rather than occurring “out of the blue”, causing a wide range of difficulties including problems in the following areas:
- Difficulties with experiencing and managing feelings including intense anxiety, sadness, suicidal thoughts, anger, eating disorders, self-harm and substance misuse and sexual difficulties.
- Difficulties with changes in consciousness such as nightmares, flashbacks and intrusive thoughts as well as forgetting traumatic events or having episodes of feeling detached from your thoughts or body (dissociation).
- Difficulties with self identity and the way in which you see yourself. People often describe feeling helplessness, shame, guilt, stigma and a sense of being different to other people.
- Difficulties with relationships including difficulties with trust, assertiveness and in managing relationships with others.
- Difficulties with health (somatisation). People who have experienced repeated traumatic events often have physical health difficulties including chronic pain, migraines, seizures, chronic fatigue or other long-term health problems.
- Difficulties with systems of meaning: Experiencing repeated traumatic events from an early age can interfere with a person’s ability to find meaning in life and can lead to feeling hopeless, helpless, empty, despairing or living with chronic suicidal thoughts.
Treatment
Complex PTSD is likely to take longer to resolve and you are likely to be referred to a mental health professional to help with your recovery. Treatment is usually carried out in three phases. The first phase involves helping you to manage your current symptoms in the here and now and is referred to as developing safety and stabilisation. If you are still being affected by trauma memories, you may then go on to talk about your experiences in more detail. This phase acknowledges the losses that have occurred as a result of the trauma, including lost opportunities and relationships. However, it is important to note that improvement is possible without talking in detail about the past if you do not wish to. Phase three involves helping you to connect with people, places and activities that may help you to continue to feel better.
Caring for somebody
Caring for somebody who has experienced complex traumatic experiences (traumatic experiences which occur repeatedly over time and usually within an interpersonal context for example childhood sexual abuse, domestic violence, as well as victims of persecution, torture and trafficking) can be difficult as they may have a number of concerning difficulties over a long period of time including difficulties managing their emotions, self-harm, depression, eating disorders, difficulties within relationships as well as flashbacks, nightmares and anxiety. Caring for friends or relatives who struggle with their mental health can have a negative impact on your own health and it is important to look after yourself.
What Helps with Post Traumatic Stress Disorder
It is normal to experience upsetting and confusing thoughts after a traumatic event, but for most people this will improve naturally over a few weeks. Most people are unlikely to require access to specialist mental health care.
You should visit your GP if you or someone you know is still having problems about four weeks after the traumatic experience, or if the symptoms are particularly troublesome.
Your GP will want to discuss your symptoms with you in as much detail as possible. They will ask whether you have experienced a traumatic event in the recent or distant past and whether you re-experience the event through flashbacks or nightmares.
Your GP can refer you to mental health specialists if they feel that you would benefit from treatment.
Treatments
The main treatments for post-traumatic stress disorder (PTSD) are psychological therapy and medication
Traumatic events can be very difficult to come to terms with, but dealing with your feelings and thoughts and seeking professional help has been shown by research to help in the treatment of PTSD. It is possible for PTSD to be treated many years after the traumatic event occurred which means that it is never too late to seek help.
Watchful waiting
If you have mild symptoms of PTSD, or if you have had symptoms for less than four weeks, an approach called watchful waiting may be recommended.
Watchful waiting involves carefully monitoring your symptoms to see whether they improve or get worse. It is sometimes recommended because 2 in every 3 people who develop problems after a traumatic experience get better within a few weeks without treatment.
If watchful waiting is recommended, you should have a follow-up appointment within one month.
Psychological therapy
If you have PTSD that requires treatment, psychological therapy is usually recommended first. A combination of psychological therapy and medication may be recommended if you have severe or persistent PTSD.
The treatment is carried out by trained mental health professionals who listen to you and help you come up with ways to help you resolve your problems. The main types of psychological therapy used to treat people with PTSD are described below.
Cognitive behavioural therapy (CBT)
Cognitive behavioural therapy (CBT) aims to help you manage your problems by changing how you think and behave. Trauma-focused CBT uses a range of psychological treatment techniques to help you come to terms with the traumatic event.
For example, your therapist may ask you to confront your traumatic memories by thinking about your experience in detail. During this process your therapist helps you cope with any distress you feel, while identifying any unhelpful thoughts. Your therapist can help you gain control of your fear and distress by changing the negative way you think about your experience. For example, feeling that you are to blame for what happened or fear that it may happen again.
You may also be encouraged to gradually restart any activities you’ve avoided since your experience, such as driving a car if you had an accident.
Eye movement desensitisation and reprocessing (EMDR)
Eye movement desensitisation and reprocessing (EMDR) involves making side-to-side eye movements, usually by following the movement of your therapist’s finger, while recalling the traumatic incident. Other methods may include the therapist tapping their finger or playing a tone.
Although it might seem a bit strange at first, there is research evidence to show that it can be effective in resolving some of the most distressing symptoms of PTSD.
Group therapy
Some people find it helpful to speak about their experiences with others who are experiencing similar difficulties. Group therapy can be used to teach you ways to manage your symptoms and help you understand the condition.
Medication
Antidepressants such as paroxetine, sertraline, mirtazapine, amitriptyline or phenelzine are sometimes used to treat PTSD in adults. A combination of medication and psychological therapy can be particularly helpful.
Living with Post Traumatic Stress Disorder
Post Traumatic Stress Disorder can make you feel unsafe and in danger even after the threat has passed. It is difficult to recover if you are still in danger. It is therefore important to identify areas in your life in which you feel unsafe and, where possible, take steps to manage these. Thinking through the areas of safety below may be helpful:
Emotional safety: Do you feel safe within your emotions? Are the ways in which you are coping with your feelings safe or unsafe: for example are you numbing or shutting off from your feelings as you fear they will overwhelm you? Are you self-harming or using substances? are you experiencing suicidal thoughts?
Relationship safety: Are the people around you supportive? Is there anyone who is taking advantage of you emotionally, sexually or financially? Do you find yourself pushing people away if they come too close? Do you find it difficult to trust people?
Physical safety: Are you looking after yourself physically? Are you eating regularly, getting enough sleep, attending regular health checks, taking regular exercise? Are you taking risks with your health?
Environmental safety: Is the area you live in safe? Do you feel afraid to go out? Did the traumatic event/s occur at home and you are constantly reminded of it? Or is the trauma still happening at home or nearby?
A mental health professional can help you identify areas of risk in your life and create a safety plan to manage these.
Psychoeducation: Finding out more about the impact that trauma has on the brain can be very helpful. Understanding that your symptoms are not a sign of “being weak” but rather your body and your brain trying to process, cope with and heal from what happened can be very powerful. It can be helpful for a mental health professional to help you understand how trauma is affecting you. There is an information booklet from NHS Inform about how to cope with PTSD.
Managing nightmares and flashbacks: Understanding why and how nightmares and flashbacks occur can help you feel more in control of your symptoms. Although they can be intensely powerful and distressing at the time, it is important to remember that they will pass. Identifying your specific triggers can be helpful in making you feel more in control again. Even if you feel that they occur “out of the blue” there may be subtle cues or reminders of the traumatic event such as a specific feeling or piece of music or smell which set them off.
Grounding: Flashbacks can make you feel as if the danger is still here. Grounding helps focus your attention on one very specific thing at a time, pulling you back into the here and now. For example, smelling a strong, pleasant smell such as peppermint or lavender oil, identifying five things you can hear, touch or see, picking up an object and studying it intently using all your senses to describe it. Some people find it helpful to make a flashcard to keep with them, reminding them of the current date and time and having a “safe” word or phrase on it.
Talking or writing about what happened: Many people find that talking about what happened in a safe environment with a trusted person can help them make sense of what they have been through. This is best done with the guidance of a mental health professional.
Recovery from PTSD can take time. It is important to look after your physical health in the meantime by ensuring you are eating and drinking regularly and keeping physically active.
Looking after someone with…Post Traumatic Stress Disorder
Following a traumatic event
Immediately after a traumatic event the most important thing is to ensure that a person is safe from further danger and that their physical needs are taken care of including medical treatment if required. It is important for you to be guided by the person’s wish to talk. If they want to talk, be present and listen to them, providing comfort and consolation. Don’t pressure them to talk if they don’t want to. Encourage them to seek support from friends and family and point them towards information which explains that it is natural and normal to be upset and distressed at this time. Flashbacks, nightmares, an increased sense of threat and avoidance are normal in the early stages and most people will recover without needing further help. Encouraging people to keep to a gentle routine and look after themselves is important. However, if you become concerned that someone’s symptoms are not resolving after a month or that their distress is intense then urge them to seek help through their GP.
Coping with flashbacks
If you are with somebody whilst they are experiencing a flashback it can be helpful to “ground” them in the here and now. This means gently bringing them into the present by asking them to use their senses to describe what they can see, hear, or feel in the present moment. Smell is a very powerful way of doing this. You can encourage the person to keep some favourite perfume or essential oil to hand. You can ask them to state their name, age and the current date and name three things they can see, feel and hear. Alternatively, you could ask them to hold an object such as a stone and describe it in great detail. Find out more about grounding techniques.
Managing a disclosure of other forms of trauma
If somebody discloses a traumatic event to you such as domestic violence or childhood sexual abuse it is important to listen and acknowledge what they are telling you. Hearing accounts of abuse can be distressing and confusing, particularly if it brings up issues for yourself. It is important that the person feels that they have been listened to and believed. Try to focus on them and how they must be feeling rather than your own response and gently encourage them to seek help if they want to. They can do this by contacting their GP in the first instance.
Complex PTSD
Caring for somebody who has experienced complex traumatic experiences (traumatic experiences which occur repeatedly over time and usually within an interpersonal context for example childhood sexual abuse, domestic violence, as well as victims of persecution, torture and trafficking). You can read a description of what Complex PTSD is. It can be difficult as they may have a number of concerning difficulties over a long period of time including difficulties managing their emotions, self harm, depression, eating disorders, difficulties within relationships as well as flashbacks, nightmares and anxiety. Caring for friends or relatives who struggle with their mental health can have a negative impact on your own health and it is important to look after yourself.
Further information for carers is available on the NHS Greater Glasgow and Clyde carers site
Further Information and Support
Archway Glasgow – provides services and support to men and women aged 13 and over who have experienced rape or sexual assault within the past seven days.
Call: 0141 211 8175
Assist – provides advocacy, information and support to women and men whose partners or ex-partners are appearing in Glasgow’s domestic abuse court.
Call: 0141 276 7710
Breathing Space – free confidential phoneline you can call when you are feeling stressed or down.
Call: 0800 83 85 87
Childline – free national helpline for children in trouble or danger. It provides a confidential phone and online counselling service for any child 24 hours a day.
Call: 0800 11 11
Combat Stress is a military charity specialising in helping ex-servicemen and women. If you are serving or have served in the UK armed forces they run a 24 hour helpline.
Call: 0800 138 1619
CRUSE is a UK charity providing support and information for people who have experienced bereavement. They run a support helpline.
Call: 0845 600 2227 (calls costs up to 8p per minute, plus your phone company’s access charge per minute)
Rape Crisis – is a UK charity providing a range of services for people who have experienced abuse, domestic violence and sexual assault. They run a free helpline service every day from 6pm-midnight
Call: 0808 8010302
The Anchor, Glasgow Psychological Trauma Services. This is a specialist mental health service within NHS Greater Glasgow and Clyde for people experiencing complex PTSD. Referrals can be made by GPs or other health and social care professionals
Scottish Women’s Aid provide help and support to female survivors of domestic abuse. You can phone the domestic abuse helpline
Call: 0800 027 123
Victim Support provides support and information to victims or witnesses of crime.
Self Help Resources
There are individual self-help guides from Get Self help about PTSD and Flashbacks
BSL – Post Traumatic Stress Disorder
NHSGG&C BSL A-Z: Mental Health – Post Traumatic Stress Disorder
Post-traumatic stress disorder (PTSD) is a type of anxiety disorder which you may develop after being involved in, or witnessing, traumatic events. A traumatic event is one where you are in danger, your life is threatened, or where you see other people dying or being injured. Examples of traumatic events include road traffic accidents, assaults and sexual assaults, being involved in a natural disaster such as an earthquake, witnessing or experiencing war, torture or being held hostage.
It is usual for a traumatic event to cause upset and distress. Most people will recover with the support and care offered by family and friends and by using the ways of coping that they would normally use to deal with stress. However, some people will experience distress that is more intense and longer lasting and may result in Post Traumatic Stress Disorder (PTSD). Symptoms of PTSD include nightmares relating to the event, avoidance of things that may remind the person of the trauma, flashbacks, feeling on edge and always on the lookout for danger and negative changes in mood and thought.
NHSGG&C BSL A-Z: Mental Health – Trauma
The situations we find traumatic can vary from person to person. There are many different harmful or life-threatening events that might cause someone to develop PTSD. A traumatic event is one where you see that you are in danger, your life is threatened, or where you see other people dying or being injured.
Please note that this video is from a range of BSL videos published by NHS Greater Glasgow & Clyde
Was this helpful?
It is normal in our lives that things or situations can sometimes make us feel scared or afraid. Sometimes we can even feel scared of things that we know do not actually cause us a real threat. Common things that people are scared of include spiders, snakes, needles, heights, small or enclosed spaces, flying, and being in busy environments.
A phobia is more pronounced and more intense than a simple fear of an animal, object, place, or situation. When someone has a phobia, their life can become so disrupted that they are unable to go into particular situations or to come across particular objects. A phobia is a type of an anxiety disorder. You may find it helpful to read more about Anxiety and other anxiety disorders such as Generalised Anxiety Disorder and Panic Disorder
More Information
Signs and Symptoms of Phobias
When you or someone you know has a phobia, the anxiety can feel so intense that you may fear coming into contact with the thing that makes you feel anxious. You may find that you either avoid situations that you fear or you become extremely anxious in them. When someone has a phobia of something, they often notice changes to their thoughts (for example, noticing frightening thoughts such as “this is extremely dangerous”), their emotions (for example, feeling extremely anxious), and their behaviours (for example, taking precautions to avoid coming into contact with the feared thing).The fear is often so strong that it can impact on your day to day life.
If you have a phobia, you may also experience anxiety if you believe that you may come into contact with the feared situation or object. In some cases, you may find that you experience anxiety even when thinking about the thing that you are scared of. For example, if you have a phobia of spiders (arachnophobia), you may feel anxious when you come into contact with a spider, when you see a photo of a spider or when you think about a spider. You may also have thoughts that pop into your mind about spiders without trying to think about spiders. These are sometimes called “Intrusive thoughts”. Sometimes, your anxiety might lead to the experience of panic attacks. In addition, you may experience a number of unpleasant physical symptoms such as:
- Racing heart rate
- A sensation of a “thumping heart” (palpitations)
- Difficulty breathing or fast breathing
- Feeling sick or nauseous
- Dizziness or feeling lightheaded
- Trembling or shaking
- Sweating
- Dry mouth
- Chest feels tight or painful
- Confusion
- “Butterflies” in the stomach
- Feeling restless
- Tingling or numbness in toes and/or fingers
- A sudden need to use the toilet.
If you do not often come into contact with the animal, object place or situation that is the source of your phobia, it may not have as much impact on your day to day life. However, if you have agoraphobia (extreme fear of open or public places), it may seem much more difficult to live your life day to day. People who have a phobia can often also experience other mental health difficulties such as other anxiety disorders and depression.
Types of Phobias
There are two types of phobias. These are specific and complex phobias.
A Specific Phobia is a fear of a single object, situation or activity. These phobias often develop when a person is a child or an adolescent. For many people, these phobias can lessen as they grow older.
There are many different types of specific phobias. Some of the most common ones are:
- Animals (such as dogs, insects, snakes, and rodents)
- The environment (such as heights, water, and darkness)
- Situations (such as flying, visiting the dentist, medical interventions, and tunnels)
- Body-based phobias (such as blood, vomit, choking, injections, and injury).
A Complex Phobia is one that involves multiple anxieties. These phobias, therefore, tend to have more of an impact on a person’s day to day life. They also tend to develop when someone is an adult. Common complex phobias include:
- Agoraphobia: This is a fear of situations such as open spaces, travelling alone, busy environments and public environments. If you experience Agoraphobia, you may find that you fear going into situations where it would be difficult to leave or escape to somewhere safe, such as your home. This can lead to someone with Agoraphobia avoiding a lot of situations which can include leaving their house, using public transport, being in lifts or going to busy shops. Often people who experience Agoraphobia can find it difficult to seek help and support as they find it difficult to visit their GP surgery or to leave their home for appointments.
- Social Phobia: If you have a Social Phobia, you may have a fear of situations that are social or involve some kind of performance, such as a party or public speaking. A lot of people can find social situations difficult and they may feel shy or awkward. That is a very normal way to feel. If you have a Social Phobia, there will be a more intense feeling of fear or dread, and you may find that you often try to avoid these situations. If you experience Social Phobia, you may worry that the way you act may seem unacceptable or embarrassing to others, or you may be worried about being judged negatively. Sometimes people who experience Social Phobia can find it very difficult to seek support as they find it difficult to phone or meet people who might be able to help them.
What Helps
There is now a lot of research which has helped us to understand what can help someone who is experiencing a phobia. There is also evidence that many phobias can be successfully treated. Sometimes, a person will decide that they do not want to or feel unable to address their phobia. These individuals may take a lot of care to ensure that they avoid the situation or object that they fear.
Without treatment, people can develop what we call “safety behaviours”, such as avoiding drawing attention to themselves, planning ways to escape feared situations, or avoiding the feared situation or object. While these behaviours are understandable and may make you feel that you are keeping yourself safe, these behaviours actually help to maintain the phobia and can make it worse over time. Often, treatments focus on helping the person to understand their phobia, reduce their use of their safety behaviours and learn more helpful ways of coping with their anxiety. This is done in a way and at a pace that is agreed with the person experiencing the phobia.
If you would like to access treatment for your phobia, the first place you would normally visit is your GP surgery. Your GP should explain all of your options to you and your views should be considered before choosing any treatment. There are three main treatments that are most frequently recommended:
- Self-help materials;
- Psychological or talking therapies; and
- Medication.
Self-help Material
There are individual self help courses and materials that you may find online or that your GP may direct you to. These can help you to better understand your phobia. These materials also often recommend ways to manage or cope with phobias. As a result, the aim of these materials is to help you to take the first steps towards managing your phobia. Your GP may also refer you to self-help groups where you can learn more about phobias with other individuals who are experiencing phobias. There are a lot of resources available that can explain phobias and describe ways of managing them.
Psychological or Talking Therapies
Talking therapies can help people with phobias. A healthcare professional will often meet with you for one hour each 1-2 weeks to help you to develop ways of coping with and managing your phobia. The talking therapy shown to have the best effectiveness with phobias is Cognitive Behavioural Therapy (CBT). CBT involves helping you to look at and challenge some of your thoughts which may be making you feel anxious and fearful of the specific situation or object. Therapy can also help you to learn new ways of dealing with the phobia. Your GP might refer you to a Cognitive Behavioural Therapist, a Mental Health Practitioner, or a Clinical Psychologist to help you with this. You can read more about Cognitive Behavioural Therapy.
Medication
If you prefer not to try talking therapies or self-help materials, or if you continue to struggle with your phobia, your GP may discuss medication options with you. Antidepressant medications are commonly used when people experience depression. However, sometimes they also help to reduce the symptoms of phobias, particularly agoraphobia and social phobia, even if you are not depressed. Sometimes GPs will prescribe these to help with phobias. It is important to remember that these do not work straight away and can often take two to four weeks before people notice a change. If you visit your GP to discuss your phobia, they may also recommend benzodiazepines such as Diazepam. These often reduce symptoms of phobias and anxiety. However, they are addictive, can make you feel drowsy, and can stop being as effective after a few weeks. As a result, they are not a useful long term treatment for phobias.
Living with…Phobias
If you or someone you know is living with a phobia, you may notice an impact on their day to day life. A phobia can make it very difficult for a person to live their life the way they used to or the way that they would like to. If you have a phobia, you may experience significant distress and anxiety when you come into contact with the object or situation that you fear. You may also experience anxiety if you believe that you may come into contact with the feared situation or object. In some cases, you may find that you experience anxiety even when thinking about the source of your phobia.
Sometimes, the impact that a phobia can have on a person’s life can depend on the type of phobia. If you do not often come into contact with the animal, object place or situation that is the source of your Specific Phobia, it may not have as much impact on your day to day life. However, if you have a Complex Phobia such as agoraphobia or social phobia, it may seem much more difficult to live your life day to day.
Looking after someone with…Phobias
Witnessing someone close to you living with a phobia can be very difficult to see. It can be hard to know how to support a family member or a friend with any type of anxiety disorder. It can also be difficult to see the impact it might have on their daily life, including a possible effect on their work or how they interact with other people.
If you are trying to care for or support someone with a phobia, it is important to be supportive and sympathetic to what they are going through. Sometimes you might find it difficult to understand why they are so afraid of the source of their fear. It may not make sense to you. However, it is important to remember that their fear and anxiety is real. Individuals who experience phobias can find it distressing if they believe others do not understand them or do not take their difficulties seriously.
When reading about phobias, you may learn that avoiding situations or objects can make a phobia worse over time. Sometimes, this might lead you to want to push your family member or friend to face their phobia. It is important to remember not to put pressure on the person who is experiencing the phobia to do any more than they feel ready to do. It can be very distressing for the person to be forced to do more than they feel comfortable doing. Instead, it might be helpful to ask your family member or friend if there is anything you can do to help. This might be things such as talking to them calmly about how they are feeling or doing slow, calming breathing exercises with them.
You may also find that you can support your friend or family member by encouraging them to seek treatment for their phobia. This might mean supporting them to visit their GP or a therapist, or providing them with some information that you have found about phobias. Remember, it will be up to the person with the phobia to decide when they feel ready to seek help from services.
Further information for carers is available on the NHS Greater Glasgow and Clyde carers site.
Further Information and Support
If you would like further information on phobias, you might find the following websites helpful.
NHS Choices website provides further information on phobias including symptoms, causes and treatments, as well as the real life stories of people who have experienced a phobia.
Centre of Clinical Interventions also has some self-help workbooks that you can work through yourself
MIND also provides a booklet which gives information about phobias, including how to support someone experiencing a phobia.
Anxiety UK, No Panic and Triumph over Phobia are other online resources developed to help and support individuals who experience phobias and other anxiety disorders.
GP surgeries also often offer leaflets or booklets on a number of mental health difficulties including phobias. They sometimes also offer information on treatments such as psychological therapy.
Acknowledgements
Understanding Phobias (2014) © Mind. This information is published in full at mind.org.uk
Phobias – what, who, why and how to help? (2008) © British Psychological Society
BSL – Phobias
A phobia is a type of anxiety disorder. It is an extreme form of fear or anxiety triggered by a particular situation (such as going outside) or object (such as spiders), even when there is no danger. For example, you may know that it is safe to be out on a balcony but feel terrified to go out on it or even enjoy the view from behind the windows inside the building. Likewise, you may know that a spider isn’t poisonous or that it won’t bite you, but this still doesn’t reduce your anxiety.
Someone with a phobia may even feel this extreme anxiety just by thinking or talking about the particular situation or object
Please note that this video is from a range of BSL videos published by NHS Greater Glasgow & Clyde.
Was this helpful?
In the same way that we all have physical health we also all have mental health. In much the same way as we experience ups and downs in our physical health, we can also face ups and downs in our mental health. We are all vulnerable to experience times in our life when we struggle to maintain a sense of balance and well-being which causes us to experience mental health issues. This can also be true in pregnancy where all women experience perinatal mental health – both good and not so good.
When it’s not so good it can also be known as ‘perinatal mental health problems’, ‘perinatal mental illness’ or ‘depression and anxiety in the perinatal period’.
It is important to know that there is always someone you can turn to for help and support and it’s ok to tell your midwife/GP/health visitor if you’re struggling.
Pregnancy can be both an exciting and worrying time for parents-to-be. Pregnant women experience a range of physical and emotional changes, all of which may trigger low mood or anxiety. It’s completely normal to feel excited about your pregnancy but also have moments of feeling worried or scared. Pregnancy – and having a baby – is life-changing so it’s natural to experience a range of feelings including low mood or anxiety. Try making some small changes in your life, such as taking some time out for yourself to relax, talking about your problems or getting more rest or sleep, can usually improve your mood. The good news is that low mood will tend to lift after a few days or weeks.
Low mood and anxiety during or after pregnancy doesn’t necessarily mean that you have perinatal depression. However, if you feel that your condition is worsening and suspect that it may be progressing to depression, it is important to speak to your GP or Midwife. Signs of this happening include more frequent bouts of low mood, finding it difficult to improve your mood and the inability to feel happy.
Up to one in five women and one in ten men are affected by mental health problems during pregnancy and the first year after birth. Unfortunately, only 50% of these are diagnosed. Without appropriate treatment, the negative impact of mental health problems during the perinatal period is enormous and can have long-lasting consequences on not only women, but their partners and children too. However, this is not inevitable. When problems are diagnosed early and treatment offered promptly, these effects can be lessened.
Sometimes there is an obvious reason for low mood and anxiety during or after pregnancy, but not always. You may feel distressed, or guilty for feeling like this, as you expected to be happy about having a baby. However this can happen to anyone and it is not your fault.
It’s never too late to seek help. Even if you have low mood or anxiety or have been depressed for a while, you can get better. The help you need depends on how severe your illness is. Mild symptoms can be helped by increased support from family and friends.
If you are more unwell, you will need help from your GP and health visitor. If your Low mood or anxiety is prolonged and severe, you may need care and treatment from a mental health service.
Myths about Perinatal mental health
Perinatal depression is often misunderstood and there are many myths surrounding it. These include:
- Perinatal depression is less severe than other types of depression. In fact, it’s as serious as other types of depression.
- Perinatal depression is entirely caused by hormonal changes. It’s actually caused by many different factors.
- Perinatal depression will soon pass. Unlike the “baby blues”, perinatal depression can persist for months if left untreated. In a minority of cases, it can become a long-term problem.
- Perinatal depression only affects women. Research has actually found that up to 1 in 25 new fathers become depressed after having a baby.
When does Perinatal mental health occur?
The timing varies. About a third of women with Perinatal mental health have symptoms which started in pregnancy and continue after birth. Post Natal Depression often starts within one or two months of giving birth.
Acknowledgement: Royal College of General Practitioners Perinatal Mental Health Toolkit
More Information
What is Perinatal Mental Health?
Around 1 in 10 women will experience postnatal depression after having a baby. However depression and anxiety are equally as common during pregnancy. Most women recover with help from their GP, health visitor and midwife, and with support from family and friends. However severe depression requires additional help from mental health services.
The symptoms of postnatal depression are similar to those in depression at other times. These include low mood, sleep and appetite problems, poor motivation and pessimistic or negative thinking.
Two in 1000 women will experience postpartum psychosis. The symptoms of this illness can come on quite rapidly, often within the first few days or weeks after delivery, and can include high mood (mania), depression, confusion, hallucinations (odd experiences) and delusions (unusual beliefs). Admission to a Mother & Baby Unit (MBU) is advised for most women, accompanied by their baby. Women usually make a full recovery but treatment is urgently necessary if symptoms of postpartum psychosis develop.
What helps
The following advice on how it feels to be unwell and what was, and what was not, helpful, is from a member of the Maternal Mental Health Scotland (MMHS) change agents, people with lived experience of Post Natal Depression (PND). This member had PND after having their daughter two years previously. They were also diagnosed with anxiety & depression which was noted as potentially sparked from suffering from PND.
“What does it feel like to be unwell – uncontrollable, lonely, crazy, low, tired, lack of energy. The only way I could describe it, is to say how low and crazy I felt. I felt when everything went right and my baby was “settled” I had a great day but as soon as we had an unsettled day, the smallest thing would set me off into a downer of a mood that I felt I couldn’t shift. It felt like someone was controlling my mind and body and I was in a deep hole I couldn’t get out of. Horrendous and sad feeling. I had so much support and amazing family around me yet I pushed them all away and wanted no one.
“What was helpful ” – speaking to people I wasn’t close to. Finding a really helpful & understanding doctor who would take the time out and listen to my true feelings and understand the severity. Speaking to other mums who were going through the same & also advising my family on my feelings.
“What was not helpful ” – the first doctor I got tried to put it down to baby blues when I KNEW there was something wrong. I was told that having PND, it isn’t that common you would pick the problem up by yourself. I was in tears and broke down explaining that I isn’t want my baby anymore, I wanted to get in my car and drive as far away as possible and never come back, I wanted a different life.”
Living with…Peri-Natal Depression
For patients
Mental health in pregnancy and the postnatal period
- SIGN Guidelines: Patient Information
- RCPsych: Mental health information on perinatal disorders
- Action on Postpartum Psychosis: Insider Guides
For professionals
Resources for healthcare staff
- Maternal Mental Health Scotland
- NSPCC Scotland & Maternal Mental Health Scotland: Getting It Right for Mothers and Babies-Closing the gaps in community perinatal mental health services
- LSE & Maternal Mental Health Alliance: Costs of perinatal mental health problems
- Everyone’s Business: Maternal Mental Health
Looking after someone with…Perinatal Depression
Involvement of partners and significant others
We will ask for your consent before sharing any information with friends, family members and carers.
Further information for carers is available on the NHS Greater Glasgow and Clyde carers site
Carers support
A carer is someone who looks after a partner, relative or friend who cannot manage without help because of illness, frailty or disability. They may or may not live together.
If you would benefit from support in your caring role, local carers services can help. They can provide you with help and support regarding a number of issues including access to respite, short breaks, information and advice on a wide range of topics, emotional support and access to carers support groups. To find information about your local carers service anywhere in Scotland please contact
The Carers Information Line
Telephone: 0141 353 6504
Email: info@glasgowcarersinformation.org.uk
Support for young people
- YoungMinds is a leading UK charity committed to improving the emotional well being and mental health of children and young people.
- Baby Buddy, urgent access to mental health services – available 24 hours per day
- Working hours: Your GP can refer you to the local Community Mental Health Team (CMHT) or Crisis Intervention Team
- Out of hours: Call NHS 24 on 111
- Bluebell PND service Glasgow – 0141 221 1535
- Crossreach
- Home Start Glasgow North – 0141 9482289, email info@homestartglasgownorth.org.uk
- NHSGGC Perinatal Mental Health Service
Your Midwife, GP and Health Visitor can offer support and advice.
BSL – Peri-Natal Depression
Postnatal depression (PND) affects around 10% of mothers. This is much more serious than the period post birth known as ‘baby blues’ which usually lasts between one to three days. PND can develop slowly and may not be noticeable until several weeks after the baby’s birth, or may continue on from the baby blues period. The symptoms of postnatal depression are similar to those in depression at other times. These include low mood, sleep and appetite problems, poor motivation and pessimistic or negative thinking. It can have a significant impact on the health and wellbeing of the mother and the child.
Please note that this video is from a range of BSL videos published by NHS Greater Glasgow & Clyde.
BSL – Postpartum Psychosis
NHSGG&C BSL A-Z: Mental Health – Post-Partum Psychosis
It is a severe episode of mental illness which begins suddenly in the days or weeks after having a baby. Symptoms vary and can change rapidly. They can include high mood (mania), depression, confusion, unusual experiences and strange thoughts. Postpartum psychosis is a psychiatric emergency. You should seek help as quickly as possible.
Postpartum psychosis can happen to any woman. It often occurs ‘out of the blue’ to women who have not been ill before. It can be a frightening experience for women, their partners, friends and family. Women usually recover fully after an episode of postpartum psychosis.
It is much less common than Baby Blues or Postnatal Depression. It occurs in about 1 in every 1000 women (0.1%) who have a baby
Please note that this video is from a range of BSL videos published by NHS Greater Glasgow & Clyde
