Your health
Pregnancy is a great opportunity for change and stopping smoking is the best thing you can do for your baby
Here you will find information to help you if you are thinking about stopping smoking or vaping, or if you want to help or encourage someone you know to stop smoking.
We are not here to tell you all the bad things about smoking as you already know what they are.
We are here to help, advise, encourage, motivate and support you at every step of your journey. We will tailor a unique programme for you and support you in that programme. And if you don’t succeed at first, we will not judge or criticise. We will help you to review what you have achieved and will continue to work with you until you succeed. There is also support available to help you and your family and friends too.
Many people can quit on their own, but evidence shows you are three times more likely to successfully quit and stay smoke-free by quitting with our help.
With your determination and commitment, and our encouragement and support, we are confident you can be smoke-free.
£220 Financial Incentives
Most smokers want to quit. They know it’s bad for their health and their baby. They know it is costing them greatly but cigarettes were designed to make quitting difficult. If there was something we could do to make it easier to stop smoking – shouldn’t we?
Financial incentives in pregnancy are one the most effective ways of helping women to quit and remain quit post-partum. Women receiving incentives are more than twice as likely to quit compared to those not receiving incentives.
Are you pregnant and want to stop smoking?
The Quit Your Way Pregnancy Service offers financial incentives in the form of e-vouchers that can be used at various supermarkets worth up to £220.
Earn your first £40 just by attending your telephone stop-smoking appointment and give your quit a go for seven days.
Please click the blue button below to download the incentives leaflet for more information.
What happens when a pregnant women smokes
When you smoke, your baby does too. Every cigarette contains 4,000 chemicals, which go into your lungs when you smoke. Once in your lungs, the nicotine, poisons and carbon monoxide cross the placenta to your baby. This affects baby and restricts the amount of oxygen the baby gets.
How Smoking harms your baby
Every time a pregnant mum smokes it affects her baby’s growth and development and causes her baby’s heart to beat harder.
Continuing to smoke during pregnancy increases the risk of:
• Miscarriage
• Stillbirth
• Low birthweight
• Premature birth
• Baby having a cleft lip/palate
Smoking when pregnant can also affect your child as they grow up. Babies and children whose mothers smoke during pregnancy are also at great risk of:
• Sudden Infant Death Syndrome (SIDS)
• Colic
• Infections in the airways
• Ear infections
• Asthma
• Conditions such as ADHD (attention deficit hyperactivity disorder).
• Psychological problems in childhood: disruptive behaviour and poor educational performance
Stopping smoking will help you and your baby immediately. When you stop smoking, it only takes 24 hours for the poisonous gas carbon monoxide to clear from your bloodstream. Your baby will quickly start getting more oxygen through the placenta and you will instantly start to reduce the risk of complications in your pregnancy and during baby’s birth.
Carbon Monoxide and your baby
Carbon monoxide (CO) is a colourless, odourless and tasteless poisonous gas. You can’t see it or smell it, but it is in cigarette smoke. CO is also in faulty gas boilers, car exhaust fumes, burning coal, wood, oil.
If you are exposed to carbon monoxide: the CO replaces some of the oxygen going into your lungs and gets into your bloodstream. This prevents the red blood cells from carrying oxygen around your body and to your baby. It is dangerous because it deprives the baby of oxygen, slows the baby’s growth and development, and increases the risk of miscarriage, stillbirth and sudden infant death syndrome (SIDS).
CO Breath test: NHSGGC offer CO testing to all pregnant women at their first booking appointment and subsequent appointments to show how much of this gas you and your baby have been exposed to.
Second hand smoke
Second hand smoke can affect you and your baby before and after their birth. More than 80% of second hand smoke is invisible and doesn’t smell.
Exposure to second hand smoke can increase the risk of:
• Premature birth
• Low birth weight
• Sudden Unexplained Death in Infancy (SUDI)
Babies whose parents smoke are also more likely to be admitted to hospital during the first year of life, as they are more likely to develop infections that can affect their breathing, such as bronchitis and pneumonia.
If you smoke, you will find it harder to quit if someone living with you also smokes.
It doesn’t matter how careful others think they are about keeping smoke away from you. If someone smokes in your home, you and your baby still breath in the harmful poisons. Opening windows and doors or smoking in another room will not make it completely safe.
For more information on second hand smoke and making your home smoke-free, please phone 07796 937 679 or email: ggc.quityourway.pregnancy@nhs.scot
E-cigarettes / Vaping
Current research about e-cigarette use in pregnancy shows that they are significantly less harmful to health than cigarettes. If using an e-cigarette (vaping) helps you stay smoke free, this is far safer for you and your baby than continuing to smoke.
E-cigarettes are regulated in the UK but they are not currently licensed as a stop smoking aid. If you choose to use an e-cigarette to help you to quit smoking tobacco it is important to ensure you buy one from a reputable retailer to minimise the risk of harm.
You can discuss the risk and benefits of e-cigarettes with Quit Your Way pregnancy services. They can also discuss the option of using nicotine replacement therapy, which is licensed and can be prescribed to support you with your quit attempt.
Nicotine Replacement Therapy (NRT)
Many NRT products are licensed to use in pregnancy. NRT contains only nicotine and none of the damaging chemicals found in cigarettes, so it is a better option than continuing to smoke. It helps you by giving you the nicotine you would have had from a cigarette. The Quit Your Way Pregnancy Practitioner can arrange for you to have NRT during your pregnancy. This can be in the form of patches, gum, lozenges, mouth spray or an inhalator.
Inpatients: You can also access NRT during your stay in hospital, please ask your midwife if you are interested in this.
Staying Stopped after baby’s birth
Once your baby is here you may feel as though your reason for giving up smoking is over – but it isn’t! It’s still very important you stay stopped after pregnancy. Think of what you have achieved by stopping smoking during your pregnancy – you should feel so proud!
Remaining smoke-free will result in lots of health benefits for you and your baby. Think of the money you can save to spend on your baby, or on a treat for yourself.
Research shows that children of smoking parents are more likely to try smoking and become regular smokers. If you don’t want your children to smoke, it’s best to set a smoke-free example.
If you would like to talk to a stop smoking practitioner, please phone: 07796 937 679 or email: ggc.quityourway.pregnancy@nhs.scot
Next Steps….
We know that stopping smoking is not an easy thing to do on your own but we are here to help. Quit Your Way services help thousands of people in Scotland stop smoking every year. Smoking is an addiction that for most smokers is hard to quit. We are confident that with our help you can quit, and with encouragement and support make your life and the lives of those around you smoke-free.
Next steps…
You’ve already made the first step by looking through this website. The next step is to contact us and have a chat with one of our advisers!
Phone: 07796 937 679
Email: ggc.quityourway.pregnancy@nhs.scot
Was this helpful?

From here you can access a wide-range of information on child and maternity healthcare services, including guidance and support available, both in our hospitals and in the community.
Was this helpful?
Frontline Equality Assessment Tool
The Frontline Equality Assessment Tool (FEAT) has been designed to ensure that every service gets it right every time for all our patients.
Developed in response to feedback from our staff on areas where they feel NHSGGC could be doing better, the Tool also takes into account evidence from the experiences of our patients.
The FEAT focusses on assessing how we can fully meet the needs of all our patients within frontline services. It will be used by lead members of local service teams in collaboration with the Equality and Human Rights Team to look at patient flow and integration of inequalities sensitive practice.
This will involve reviewing how patient data is collected, how communication support is assessed, knowledge of protected characteristic-related issues and associated policies and protocols as well as the impact on discharge planning.
By translating the language of legislation into practical steps for staff, the FEAT offers a sense check which highlights both where there are gaps in services’ inequalities sensitive practice and where there are examples of good practice which could be replicated in other services.
William Edwards, Deputy Chief Executive, NHSGGC

“The Frontline Equality Assessment Tool is a great addition to our processes to enable us to understand and meet the needs of our patients with protected characteristics. Not only will it help us identify where we can take positive action but will also capture where good practice is underway and share across all wards and services.”
Alastair Low, Manager, NHSGGC Equality and Human Rights Team

“Equality legislation can sometimes be seen as distinct or detached from the daily interactions that are at the heart of everything we do. We want to help change that perspective. The time we spend visiting departments will strengthen our understanding of equality legislation and its role in delivering effective, efficient and inclusive services.”
Disability Discrimination Audits (DDAs)
NHSGGC has a duty to remove access barriers for disabled patients. This takes the form of Disability Discrimination Audits (DDA) which involve conducting access audits in partnership with disabled people.
In addition to DDA audits, the Frontline Equality Assessment programme also includes a rapid assessment of a physical environment with proposed enhancements reported back to our Estates and Facilities Directorate.
We are currently carrying out a range of DDAs and FEAT reviews in Acute settings which aim to identify any adaptations required.
Professor Tom Steele, Director of Estates and Facilities

“We know that some aspects of the physical environment can still present barriers for some people who use our buildings. We are committed to a programme of ongoing improvement works as well as deigning space that will act as an enabler to staff, patients, carers and visitors.”
Was this helpful?
Pregnancy Vitamins
Healthy eating is essential to keep you and your baby healthy during pregnancy. Visit Ready Steady Baby |Eating well in pregnancy for more information about healthy eating during pregnancy.
During pregnancy, some vitamins are important to take. This page will tell you more about them and how to get these vitamins for free!
You will get Free Healthy Start vitamins throughout your pregnancy from your Midwife. These supplements contain folic acid, vitamin D and vitamin C to support you and your growing baby.

Healthy Start vitamins are suitable for vegetarians and free from wheat, fish, egg, and salt.
Contain no colours, flavours or preservatives.
Not suitable for vegans due to the source of vitamin D.
For those who are taking 5 milligram of Folic Acid, your GP will prescribe this. The Healthy Start Vitamins can be taken at the same time.
Ask your midwife for more information.
Folic Acid
Healthy Start contains your recommended 400 micrograms of Folic Acid.
Folic Acid will help your baby’s spine properly during pregnancy.
Stops Neural tube defects such as Spina Bifida, which affects how the spine is formed.
During pregnancy, you need more folic acid to support your baby’s development, which is hard to get from your diet alone.
Vitamin D
Healthy Start vitamins contains your recommended 10 micrograms of vitamin D.
Vitamin D helps our body absorb calcium to keep our bones and teeth healthy.
Low vitamin D levels can cause
• Seizures in babies after birth
• Vitamin D deficiency can cause problems and pain in the bones. This will be rickets in children.
Sources of vitamin D are limited. The best source of vitamin D is the sun and dietary sources are limited.
Vitamin C
Healthy Start vitamins contain 70 micrograms of vitamin C.
• Vitamin C helps your body to absorb iron.
• Boosts your immune system.
• To help your body make collagen and protect your cells.https://www.nhsggc.scot/downloads/health-start/
More information
Your Badgernet app will contain lots of information about pregnancy including Healthy Start.
Ready Steady Baby (NHS Inform)
Your Midwife will be there to support you throughout your pregnancy and will be happy to answer any questions.
Was this helpful?
This page provides information on person-centred visiting in our mental health wards. Information about visiting in all other areas can be found on our Person Centred Visiting page.
Frequently Asked Questions
If you are the person in hospital
On admission to the ward, you will be asked about your preferences for visitors. Your family and/or significant others can also contribute to this. We will record this on a visiting form which will be kept with your care plan.
Can my children visit?
The importance of maintaining family connections with your children, when you are in hospital, is important. We will discuss this with you and your family at admission and during your hospital stay. Where possible, we will facilitate visits in a designated family area.
If you are the visitor
We have no set visiting times. This means you can be here to support your family member or friend at any time during the day. Please discuss with your family member or friend what they would like in terms of visits and what times would work best for you both, then talk to ward staff about your plans.
There may be times when visiting takes place in a communal area or visiting room, the nursing staff will advise where visiting is offered in each ward.
Should you need to access an area out with the dedicated visiting area, please speak to the nurse in charge.
Can I visit during mealtimes?
In those Mental Health wards where visiting can only take place in dining rooms, family support during mealtimes will be discussed and agreed as part of individual visiting and care plans, in conjunction with the individual, the people who matter to them and staff.
As a visitor, what safety measures do I need to follow?
To ensure a safe environment and that of yourself and others, please discuss with the nurse in charge what is safe and not safe to take into the ward. Examples of items not deemed safe are glass bottles, knifes, medications and plastic bags. Any electrical equipment should be handed into staff to be safety checked.
Can I take my family member out of the ward when I visit?
We recognise the benefits of having the opportunity to spend time with those visiting away from the immediate ward. However, there may be times when this is not possible. Please discuss this with the nurse in charge, and always let the nurse in charge know when you are going out of the ward with your family member.
Returning following time off the ward with family member
It is important for staff to know when patients have returned to the ward. This ensures that staff maintain overall safety and activity on the ward, and allows staff to plan therapeutic engagement. In addition, this provides family members with the opportunity to feedback to staff on how the visit has gone and ask any questions regarding this.
Was this helpful?
What would £100,000 pay for?
It also equates to a day’s wages for more than 700 nurses, or more than 200 hospital consultants.
Small steps, big impact
There are things we can all do to help reduce waste:
- Resist the urge to over-order medicines: Check what medicines you have at home before you re-order, and only order what you really need when you need it
- Take control of your medication: Speak to your GP, pharmacy team or nurse about reviewing your medication to make sure they are still right for you
- Know how to dispose of unused medicines: If you have medicines at home that are out of date or no longer required, return them to your local pharmacy for safe disposal.
Take control of your medication – ask for a medicines review
Contact your GP practice and ask to be referred to the GP practice pharmacy team to discuss if your prescription is still right for you.
It is important that patients check in regularly to make sure the prescription they receive is right for them.
If you receive a repeat or serial prescription, contact your GP practice and ask to be referred to the GP practice pharmacy team for a medicines review, or ask your community pharmacist for advice.
Our pharmacy teams are here to help your with your medicines, and they will work with you to make sure the medications you receive are right for you.
As well as being beneficial for your care, medication reviews help reduce medicines waste.
Medicines Waste Across NHSGGC
Mythbusters
If I don’t use my medicines, I can return them for someone else to use
Medicines cannot be reused or recycled once they have been dispensed to you.
It’s OK for me to order extra medicines so I don’t run out
Over-ordering can lead to medicines going to waste if your prescription or health needs change. Please try to order only what you need, when you need it.
I’ve been taking these for years. I must still need them
If anything has changed with your health, you may not need some of your medicines anymore. Please contact your GP practice or pharmacist to arrange a medication review.
Prescriptions are free in Scotland. They don’t cost anything
Though you are not charged for your prescription medication, it still has a cost to the NHS, and the environment. It costs £11 on average for each individual medicine dispensed across Greater Glasgow and Clyde, and around 10% of the medicines dispensed, go to waste.
Resources for Staff

Was this helpful?
The GP Out Of Hours (GPOOH) service in NHS Greater Glasgow and Clyde provides urgent care to patients when their regular GP service is closed. These services are designed to handle non-life-threatening medical issues that require attention outside regular working hours, such as evenings, weekends, and public holidays.
Current GPOOH Service
The GP Out Of Hours service has been developed as an appointment-based model, that can be accessed by phoning NHS24 on 111.
This means we can help people get the right care in the right place.
Patients can access the GPOOH service in the evenings, overnight, across the whole weekend, and public holidays by contacting NHS 24 on 111.
If you require urgent non-life threatening care after your GP has closed you should phone NHS24 on 111.
Trained call handlers at NHS24 will assess your needs and if clinically appropriate will refer you to the GP Out of Hours service.
This new system also means that, where appropriate, patients can speak to a clinician over the phone or via a virtual consultation from the comfort of their own home, meaning they don’t have to travel to an urgent out of hours care centre.
Frequently Asked Questions
What is GP Out of Hours?
The GP Out Of Hours service provides urgent primary care to patients outwith normal GP surgery hours. This includes evenings, weekends, and public holidays. This is accessed by calling NHS 24 on 111.
How do I access GP Out of Hours?
Patients can access the GPOOH service in the evenings, overnight and across the whole weekend and public holidays by contacting NHS 24 on 111.
Trained call handlers at NHS24 will assess the needs and if clinically appropriate will refer the patient to the GPOOH service.
This new system means that, where appropriate, patients can speak to a clinician over the phone or via a virtual consultation from the comfort of their own home, meaning they don’t have to travel to an urgent out of hours care centre.
Why do I have to phone NHS 24?
With all patients being channelled through NHS 24 as a first point of contact, we can ensure that people are directed to the most appropriate type of care within the right environment, at the right time.
We have a fully integrated a telephone triage system into the patient care pathway, meaning where appropriate, patients can speak to a clinician over the phone or via a virtual consultation and may not even have to travel to an urgent out of hours care centre.
Where are the GP Out of Hours Centres?
There are currently GP Out of Hours Centres at:
- Inverclyde Royal Hospital (Partial weekend cover and bank holiday.)
- New Victoria Hospital
- New Stobhill Hospital
- Royal Alexandra Hospital
- Vale of Leven (Lomond)
Will people have to travel further to attend GP Out of hours?
If you need a face-to-face appointment, you may be asked to attend a GP Out Of Hours centre outwith your local area. Those who need support travelling to a centre, patient transport can be arranged.
If you cannot travel, we also offer home visiting options.
What happens if you are not able to travel to attend an appointment?
If you cannot travel, we can also offer home visiting options and for those who need support to get to a centre and patient transport can be arranged.
Why can I not just turn up to be seen?
With all patients being channelled through NHS 24 as a first point of contact, we can ensure that people are directed to the most appropriate type of care within the right environment, at the right time.
We have a fully integrated a telephone triage system into the patient care pathway, meaning where appropriate, patients can speak to a clinician over the phone or via a virtual consultation and may not even have to travel to an urgent out of hours care centre. Over half of our consultations are now carried out remotely within your own home. This ensures you can be seen by the right clinical person for your care. Being seen in the home setting also reduces waiting times, travel time and infection control risks.
Is patient transport available to all patients?
Patient Transport is available to all patients. At time of arranging an appointment for a centre, the administrative staff will discuss travel arrangements to the centre for the patient. Any patients who indicate they don’t have transport means to travel to centre will be routinely offered patient transport. There is no charge for this service.
Can patient be accompanied on patient transport?
Carers can get the transport and child seats are also available and patient transport now includes accessibility for wheelchair users.
Is return transport to get patient home available?
Yes it is available both to and from the centre.
Was this helpful?
Why immunise?
The development of effective vaccines has led to a huge decrease in childhood deaths. The World Health Organization (WHO) states: ‘The 2 public health interventions that have had the greatest impact on the world’s health are clean water and vaccines.’
Benefits for you
As children develop they’re exposed to many risks, one of these risks being infections. Most of these will cause mild illnesses. However, despite great medical advances, infection can still cause severe illness, disability and, at times, death.
Before vaccines were available, many children in the UK died from diseases such as whooping cough, measles and polio. Despite successful immunisation programmes, the diseases that vaccines protect against do still exist.
The benefit of immunisation is that your child has the best possible protection against dangerous diseases. This can give you peace of mind.
Changes to childhood vaccinations – from 1st of July 2025
What parents and caregivers need to know
Experts regularly review the vaccination programme to make sure it gives children the best protection. New research and changes in vaccine supply mean the vaccination schedule in Scotland has changed.
If your baby was born on or before the 30th of June 2024, they will already be mid-vaccine schedule and will remain on that schedule until it is complete. There is no action required from you and your baby will be invited for these vaccinations when the time approaches.
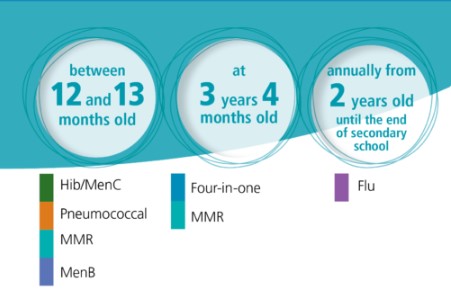
If your baby was born on or before the 30th of June 2024, they will continue to follow this schedule.
- 12-13 months – HibMenC, Pneumococcal, MMR, MenB
- 3 years 4 months – Four-in-one, MMR
- From 2 years old – Flu
The following changes came into place on the 1st of July 2025.
- 8 weeks – Six-in-one, Rotavirus, MenB
- 12 weeks – Six-in-one, Rotavirus, MenB
- 16 weeks – Six-in-one, Pneumococcal
- 12-13 months – MenB, Pneumococcal, MMR
- 18 months – Six-in-one, MMR
- 3 years 4 months – Four-in-one

If your child turned one year of age on or after 1 July 2025 (DOB on or after 1 July 2024), they will pick up on this schedule from here:
- 12-13 months – MenB, Pneumococcal, MMR
- 18 months – Six-in-one, MMR
- 3 years 4 months – Four-in-one
What’s changing?
Some vaccines will now be given at different times, and a new appointment will be added when your child is 18 months old.
Who decides this?
The changes are based on advice from the Joint Committee on Vaccination and Immunisation (JCVI) – a group of independent experts who guide the UK and Scottish vaccination programmes.
What happens next?
There is no action required from you. You’ll be given clear information when it’s time for your child’s next vaccinations.
Why is this important?
Vaccines are the best way to protect your child from serious illnesses. These updates help make sure the programme stays safe, effective, and up to date.
Changes to the routine childhood vaccination schedule
Changes to the routine childhood vaccination schedule from 1 July 2025 and 1 January 2026
Changes to be implemented
Phase 1 (from 1 July 2025)
MenB vaccination will now be offered from 12 weeks (previously 16 weeks).
- Following a recent clinical study and a review of the epidemiology, the JCVI has advised bringing forward the second dose of the MenB vaccine to provide earlier protection against this serious and sometimes fatal infection.
- Meningococcal serogroup B is responsible for the majority of UK invasive meningococcal disease (IMD) cases. Since the introduction of the routine MenB vaccination programme, peak age of infection has shifted from 5 to 6 months to 1 to 3 months of age. A substantial proportion of cases were occurring before infants gained protection from their second dose of vaccine given at 16 weeks. The change in epidemiology of IMD means it would be beneficial to move the second dose of MenB vaccine to 12 weeks of age to provide earlier protection.
- Although previously an 8-week interval between doses of MenB vaccine was recommended, evidence from a recent study showed a good response was made when the 2 doses were given 4 weeks apart.
Pneumococcal vaccination will now be offered from 16 weeks (previously 12 weeks).
- To avoid increasing the number of injections at the 12-week appointment, the first dose of the pneumococcal vaccine will be moved to the 16-week appointment.
- The change is unlikely to be clinically significant.
The Hib/MenC vaccine (Menitorix) will no longer be available.
- The manufacturer has ceased production of Menitorix vaccine. There is no other Hib/MenC vaccine available on the UK market.
- Children turning one year of age on or after 1 July 2025 (date of birth on or after 1 July 2024) will not have received the combined Hib-MenC vaccine (Menitorix) when they are invited for their 12-month vaccination appointment (they should still receive the other vaccines due at that age). These children should be offered a new 18-month routine vaccination appointment (starting from 1 January 2026) for a 4th dose of the 6-in-1 vaccine (DTaP/IPV/Hib/HepB (hexavalent)) vaccine, given alongside the second dose of MMR.
- The JCVI has agreed that protection against MenC is no longer required in this age group due to the high uptake of vaccination in the secondary school programme. Sustaining high uptake of the MenACWY vaccine, currently offered to S3 pupils, is important to maintain indirect protection.
Phase 2 (from 1 January 2026)
From January 2026, the MMRV vaccine will be offered as part of the routine childhood immunisation schedule. It replaces the MMR vaccine.
The MMRV vaccine protects against measles, mumps, rubella, and varicella (chickenpox). These are serious diseases that can be life-threatening.
Measles is a very infectious virus. It spreads easily though the air when people with the virus cough or sneeze. It can cause serious health complications, like pneumonia and encephalitis. In very serious cases, measles can be life-threatening.
Mumps is caused by a virus. It can cause permanent deafness, viral meningitis, and encephalitis. Mumps spreads through the air when people with the virus cough or sneeze, and is very infectious.
Rubella is caused by a virus. If caught in pregnancy, it can cause a miscarriage or affect the unborn baby. It can cause a condition called congenital rubella syndrome (CRS), which damages a baby’s sight, hearing, heart and brain. Rubella is spread through the air when people with the virus cough or sneeze, and is very infectious.
Varicella (chickenpox) is a highly infectious disease caused by a virus. Varicella is spread through direct contact with someone who is infected.
Read more about why your child should get the MMRV vaccine
Who can get the MMRV vaccine
The MMRV vaccine is offered to children as part of the routine childhood vaccination programme. When your child will be offered the vaccine depends on when they were born.
If your child was born on or after 1 January 2025
If your child was born on or after 1 January 2025, they’ll be offered 1 dose of the MMRV vaccine at both:
- 12 to 13 months
- 18 months
If your child was born between 1 July 2024 and 31 December 2024
If your child was born between 1 July 2024 and 31 December 2024, they’ll be offered a dose of the MMRV vaccine at:
- 18 months
- 3 years 4 months
If your child was born before 30 June 2024
If your child was born before 30 June 2024, they’ll be offered a dose of the MMRV vaccine at 3 years 4 months.
Introduction of a new 18-month appointment where the additional 6-in-1 (4th dose) vaccine will be offered.
- To replace the Hib dose, an additional dose of the 6-in-1 ((DTaP/IPV/Hib/HepB (hexavalent)) vaccine will be offered at a new routine appointment at 18 months.
- Children turning one year of age on or after 1 July 2025 (date of birth on or after 1 July 2024) will not have received the combined Hib-MenC vaccine (Menitorix) when they are invited for their 12-month vaccination appointment (they should still have received the other vaccines due at that age). These children should be offered a new 18-month routine vaccination appointment (starting from 1 January 2026) for a 4th dose of the 6-in-1 vaccine (DTaP/IPV/Hib/HepB (hexavalent)) vaccine, given alongside the second dose of MMR.
The second dose of MMRV will be brought forward from the 3-year 4-month appointment to the new 18-month appointment.
- The second MMRV dose is being moved forward in the schedule to provide earlier protection and, hopefully, help to improve uptake. Research showed moving the second dose of MMR forward in London led to higher uptake.
Queries about scheduling
My children are different ages, will they be on different schedules?
Yes your children might be on different schedules as the schedule children follow is dependent on their date of birth. When changes to vaccination programmes happen, they must be rolled out on a phased basis to ensure NHS immunisation teams are able to deliver the vaccines effectively alongside other programmes. Changes to programmes are based on the advice of the Joint Committee on Vaccination and Immunisation (JCVI). These decisions are based on several factors, including the risk of the disease and the effectiveness of the vaccine.
If I delay my child’s vaccines, will they change schedules?
The schedule your child follows is dependent on their date of birth not when they attend for vaccination. Do not delay getting your child vaccinated – they will not change schedules. It’s important that vaccines are given on time to make sure your child has the best protection possible. Delaying or missing vaccine doses can put your child at risk of serious diseases and getting vaccines when they are due is the best way to protect your child.
Pre-School Children
The 6-in-1 Vaccine
Overview
The 6-in-1 vaccine, also commonly known as the DTaP/IPV/Hib/HepB vaccine, helps protect your child against:
What’s pertussis (whooping cough)?
Whooping cough is a disease that can cause long bouts of coughing and choking, making it hard to breathe. Whooping cough can last for up to 10 weeks.
Babies under one year old are most at risk from whooping cough. For these babies, the disease is very serious and can kill. It’s not usually as serious in older children. Before the pertussis vaccine was introduced, on average 120,000 cases of whooping cough were reported each year in the UK.
What’s diphtheria?
Diphtheria is a serious disease that usually begins with a sore throat and can quickly cause breathing problems.
It can damage the heart and nervous system and, in severe cases, can kill. Before the diphtheria vaccine was introduced in the UK, there were up to 70,000 cases of diphtheria a year, causing around 5,000 deaths.
What’s tetanus?
Tetanus is a disease affecting the nervous system that can lead to muscle spasms, cause breathing problems and even kill. It’s caused when germs that are found in soil and manure get into the body through open cuts or burns.
Tetanus can’t be passed from person to person.
What’s polio?
Polio is a virus that attacks the nervous system and can cause permanent paralysis of the muscles. If it affects the chest muscles or the brain, polio can kill.
Before the polio vaccine was introduced, there were as many as 8,000 cases in the UK during the polio epidemic. Because of the continued success of the polio vaccination, there have been no cases of paralytic polio in the UK for nearly 40 years (the last case was in 1984). Polio remains a threat with poliovirus traces found in London sewage in early 2022.
Being fully vaccinated is the best way to protect against becoming ill from polio. It’s important to make sure you and your child are up to date with your vaccines.
What’s Hib?
Hib is an infection caused by haemophilus influenzae type b bacteria. It can lead to a number of major illnesses such as blood poisoning (septicaemia), pneumonia and meningitis. The illnesses caused by Hib can kill if they’re not treated quickly. Before the Hib vaccine was introduced, there were about 800 cases of Hib in young children every year in the UK.
The Hib vaccine only protects your baby against the type of meningitis caused by the haemophilus influenzae type b bacteria – it doesn’t protect against any other type of meningitis.
More about haemophilus influenzae type b (Hib)
What’s hepatitis B?
Hepatitis B (HepB) is a virus that infects the liver. Many people with HepB infection have no symptoms and don’t know they’re infected. Others have flu-like symptoms and yellowing of the skin (jaundice).
In children, HepB can persist for years and may eventually cause serious liver damage.
Why should my baby be vaccinated?
Babies can catch these serious diseases from birth, so it’s important to protect them as soon as possible.
When will my baby be immunised?
All babies are eligible for the vaccine free on the NHS.
Your baby will be offered the 6-in-1 vaccine around 8, 12 and 16 weeks of age. Your local NHS immunisation team will contact you to let you know about their arrangements for your baby’s routine childhood immunisations.
Most NHS immunisation teams run special immunisation baby clinics. If you can’t get to the clinic, contact your local NHS immunisation team to make another appointment.
Meningitis B (MenB) vaccine
Overview
The meningitis B (MenB) vaccine helps protect against meningitis and septicaemia (blood poisoning) caused by meningococcal bacteria B.
What’s meningitis?
Meningitis is inflammation of the lining of the brain and spinal cord. This causes pressure on the brain resulting in symptoms like:
- severe headache
- stiff neck
- dislike of bright light
- drowsiness
- convulsions/fits
Meningitis can progress very rapidly and can lead to:
- deafness
- blindness
- epilepsy
- learning difficulties
It can even lead to death.
What’s septicaemia (blood poisoning)?
Septicaemia (blood poisoning) is a serious, life-threatening infection that gets worse very quickly. The risk of death is higher compared to meningitis.
The signs of cold hands and feet, pale skin, vomiting and being very sleepy or difficult to wake can come on quickly.
More about meningitis and septicaemia
Charlotte’s story: meningococcal septicaemia (MenB)
Charlotte developed septicaemia (serious blood poisoning) through type B meningococcal disease (MenB) in 2010, before the MenB vaccine was introduced in the UK. Her mother Jenny talks about the impact on Charlotte and the rest of her family.
How common is type B meningoccocal disease?
MenB is now the cause of most cases of meningococcal disease in Scotland. Although this infection isn’t common, MenB is extremely serious and can lead to permanent disability and death. The meningococcal bacteria can also cause local outbreaks in nurseries, schools and universities.
Why should a baby be vaccinated?
MenB infection is most common in babies and young children. This is because their immune systems aren’t yet fully developed to fight off infection. The highest number of cases are in babies around 5 months of age. This is why the first immunisations are offered to babies younger than this and have to be given at 2 and 4 months of age.
This vaccine helps protect babies against MenB, There are other vaccines, like MenC, that protect against some other types of meningococcal infections.
Who is eligible for the vaccine?
The MenB vaccine is routinely offered to all babies at 8, 16 weeks, and 12 to 13 months.
When will a baby be immunised?
The MenB vaccine has been part of the routine childhood immunisation programme in Scotland since 1 September 2015. Your local NHS immunisation team will send you an appointment to bring your child in for their routine childhood immunisations.
Babies will be offered the MenB vaccine when they come in for their other routine immunisations at 8, 16 weeks and 12 to 13 months.
Find out how to contact your local NHS immunisation team regarding your vaccination appointment
If a baby is due their MenB vaccine, please ask your pharmacist about paracetamol for them. Fever can be expected after any vaccine but is more common when the MenB vaccine is given with the other routine immunisations at 8 and 16 weeks of age. This is why it’s recommended that babies gets infant paracetamol when getting these immunisations to prevent and treat fever.
Rotavirus vaccine
Overview
The rotavirus vaccine helps protect babies against rotavirus.
What’s rotavirus?
Rotavirus is a virus that infects the gut (tummy), causing severe diarrhoea and vomiting. Most babies get sick (vomit) or have diarrhoea at some time and recover fully after a few days. However, sickness and diarrhoea caused by rotavirus can lead to dehydration (loss of body fluids). Dehydration can be very dangerous for babies and young children and can require hospital treatment.
Before the vaccine was introduced in 2013, around 1200 babies in Scotland had to go to hospital every year with rotavirus.
Why should a baby be vaccinated?
The rotavirus immunisation protects a baby against this illness.
The most important thing you can do is have the baby immunised against rotavirus, as part of the Routine Childhood Immunisation Programme in Scotland.
In countries where babies already get the rotavirus vaccine there’s been a big drop in the number of babies and young children going to hospital because of the virus.
With lots of younger babies having the immunisation the chances of it spreading are reduced. Rotavirus causes fewer problems in older children, and it’s rare in adults.
When will a baby be immunised?
The rotavirus immunisation is offered to all babies in Scotland.
The rotavirus vaccine is normally given with the baby’s other routine immunisations at 8 weeks and again at 12 weeks of age. Your local NHS immunisation team will invite you for the vaccination, so there’s no need to book an appointment.
Pneumococcal vaccine for babies
Overview
The pneumococcal vaccine helps protect against illnesses and conditions caused by pneumococcal bacteria.
What illnesses and conditions are caused by pneumococcal bacteria?
Pneumococcal infection is caused by pneumococcal bacteria. It can cause serious illness such as pneumonia, and is one of the most common causes of meningitis (an infection of the lining of the brain).
Pneumococcal infection can cause:
- bronchitis
- ear and sinus infections
- a life-threatening infection of the blood (septicaemia)
- meningitis
- pneumonia (which can also be life-threatening).
Children under 2 years of age and children with certain health conditions have a higher chance of becoming unwell with pneumococcal infection.
How common are pneumococcal bacteria?
Up to 60% of children carry pneumococcal bacteria in the back of their nose and throat. They constantly pass these bacteria around by coughing, sneezing and close contact.
Why should a baby be vaccinated?
The pneumococcal vaccine provides some protection against meningitis caused by pneumococcal infection, and against other conditions such as severe ear infections and pneumonia caused by pneumococcal bacteria.
This vaccine doesn’t protect against meningitis caused by other bacteria or viruses.
Who is eligible for the vaccine?
Some children are at an increased risk from pneumococcal infection. All at risk children will be offered the vaccine according to the routine childhood immunisation programme. If you aren’t sure about your child’s health or need further advice, speak to your health professional.
When will a baby be immunised?
If a baby is eligible, they will be offered the pneumococcal vaccine when they’re 12 weeks old, with a booster dose given between 12 and 13 months. The pneumococcal booster dose between 12 and 13 months is usually given at the same time as the Hib/MenC, MMR and MenB vaccines.
In addition to this some children and adults aged from 2 to 64 years old, who are at a higher risk of developing a pneumococcal infection than the general population, will be offered additional pneumococcal vaccinations.
Your local NHS immunisation team will contact you to let you know about their arrangements for the baby’s routine childhood immunisations.
Hib Men C
Overview
The Hib/MenC vaccine helps protect a child against 2 of the causes of meningitis and septicaemia (blood poisoning). This vaccine will help protect the child through early childhood.
What is Hib?
Hib is an infection caused by Haemophilus influenzae type b bacteria. It can lead to a number of major illnesses such as septicaemia (blood poisoning), pneumonia and meningitis.
More about Haemophilus influenzae type b
What is meningitis?
Meningitis is inflammation of the lining of the brain and spinal cord. This causes pressure on the brain resulting in symptoms like:
- severe headache
- stiff neck
- dislike of bright light
- drowsiness
- convulsions/fits
Meningitis can progress very rapidly and can lead to:
- deafness
- blindness
- epilepsy
- learning difficulties
It can even lead to death.
What is septicaemia?
Septicaemia (blood poisoning) is a serious, life-threatening infection that gets worse very quickly. The risk of death is higher than with meningitis.
The signs of cold hands and feet, pale skin, vomiting and being very sleepy or difficult to wake can come on quickly.
Why should a baby be vaccinated?
A child will be offered a dose of the combined Hib/MenC vaccine between 12 and 13 months of age to:
- boost their protection against Haemophilus influenzae type b (Hib)
- help protect against meningitis and septicaemia caused by meningococcal group C (MenC) bacteria
The Hib/MenC vaccine doesn’t protect against meningitis and septicaemia (blood poisoning) caused by:
- meningococcal group B bacteria
- other bacteria or viruses such as pneumococcal or mumps
When will a baby be immunised?
A baby will be offered the Hib/MenC vaccine at 12 to 13 months. Your local NHS immunisation team will contact you to let you know about their arrangements for the baby’s routine childhood immunisations.
Most NHS immunisation teams run special immunisation baby clinics. If you cannot attend your appointment contact your NHS immunisation team to make another.
Find out how to contact your NHS immunisation team regarding the baby’s vaccination appointment
MMR
The MMR vaccine is given in 2 doses and helps protect against measles, mumps and rubella. Find out more about the vaccine, and when and where to get it.
Why should someone have the MMR vaccination?
The MMR vaccine helps to protect people against measles, mumps and rubella. It’s sometimes also offered to adults who missed their childhood immunisations.
Measles, mumps and rubella are highly infectious diseases. They can cause serious medical complications.
A high number of people in Scotland have had the MMR vaccine. This means there’s been a big reduction in the number of people catching these diseases.
Who is eligible for the MMR vaccine?
All babies and children in Scotland are eligible for the MMR vaccine.
They’ll be offered the MMR vaccine in 2 doses:
- the first between 12 and 13 months
- the second at 3 years 4 months
Although normally given at these times, if it’s missed, it can be given at any age.
Some young people and adults who missed out on their MMR vaccine may also be eligible, like those who are a planning a pregnancy. If you didn’t have 2 doses of the MMR vaccine as a child, you can contact your local NHS immunisation team to discuss your eligibility.
The 4-in-1 Vaccine
Overview
The 4-in-1 vaccine, also known as the DTaP/IPV or dTaP/IPV vaccine, helps protect your child against:
- pertussis (whooping cough)
- diphtheria
- tetanus
- polio
What’s pertussis (whooping cough)?
Whooping cough is a disease that can cause long bouts of coughing and choking, making it hard to breathe. Whooping cough can last for up to 10 weeks.
Babies under one year are most at risk from whooping cough. For these babies, the disease is very serious and can kill. It’s not usually as serious in older children.
Whooping cough germs can be spread from person to person through close contact.
What’s diphtheria?
Diphtheria’s a serious disease that usually begins with a sore throat and can quickly cause breathing problems. It can damage the heart and nervous system and, in severe cases, can kill.
Diphtheria germs are spread from person to person through close contact.
What’s tetanus?
Tetanus is a disease affecting the nervous system that can lead to muscle spasms, cause breathing problems and even kill.
It’s caused when germs found in soil and manure get into the body through open cuts or burns. Tetanus can’t be passed from person to person.
What’s polio?
Polio is a virus that attacks the nervous system and can cause permanent paralysis of the muscles. If it affects the chest muscles or brain, polio can kill.
The polio virus is usually spread from person to person, or by swallowing contaminated food or water.
Before the polio vaccine was introduced, there were as many as 8,000 cases in the UK during the polio epidemic. Because of the continued success of the polio vaccination, there have been no cases of paralytic polio in the UK for nearly 40 years (the last case was in 1984). Polio remains a threat with poliovirus traces found in London sewage in early 2022.
Being fully vaccinated is the best way to protect against becoming ill from polio. It’s important to make sure you and your child are up to date with your vaccines.
Why should my child be vaccinated?
The vaccine boosts the immunisations that were given to your child at 8, 12 and 16 weeks of age – boosting protection against pertussis (whooping cough), diphtheria, tetanus, and polio.
Who is eligible for the vaccine?
This vaccine’s offered to children aged over 3 years 4 months at the same time as they are offered the MMR vaccine. It’s also used for a primary course of immunisation in children over 10 years old and adults.
When will my child be immunised?
Your child will be offered the 4-in-1 vaccine at around 3 years and 4 months. Your local NHS immunisation team will contact you to let you know about their arrangements for your child’s routine childhood immunisations.
Most NHS immunisation teams run special immunisation clinics. If you can’t get to the clinic, contact your local NHS immunisation team to make another appointment.
Young people in Secondary School/not in mainstream education
HPV Vaccine – S1 to S6
What the HPV vaccine is for
Immunisation (vaccination) information in other languages
Evidence shows the HPV vaccine helps protect people from HPV-related cancers. The human papillomavirus (HPV) vaccine is offered to every S1 pupil in Scotland.
Getting the vaccine now protects you against future risks. HPV can lead to cancers like:
- head and neck cancers
- cervical cancer
- anogenital cancers – for example, anal, penile (penis) cancer, cancer of the vagina, and cancer of the vulva
The HPV vaccine also protects you against over 90% of genital wart infections.
Who can get the HPV vaccine
Every person in Scotland aged 11-13 will be offered the HPV vaccine free of charge.
You should not have some vaccines if you’ve had a confirmed serious (anaphylactic) reaction to:
- a previous vaccine
- any ingredient of the vaccine
About the HPV vaccine
The GARDASIL 9 vaccine is used in Scotland.
Gardasil 9 helps protect against 9 types of HPV.
The vaccine protects against HPV types 16 and 18, which are the cause of most cervical cancers in the UK (more than 80%). The vaccine also protects against types 31, 33, 45, 52 and 58, which cause an additional 15% of cervical cancers.
The vaccine also protects against 2 other types of HPV. These cause around 90% of cases of genital warts.
The HPV vaccine is not a live vaccine. It cannot cause HPV.
The vaccine is the safest and most effective way to protect against HPV.
How to get the HPV vaccine
You’ll be offered the HPV vaccine as part of the school-based immunisation programme. Vaccines are given by your local NHS immunisation team.
Your school will tell you when vaccination sessions are taking place.
Find out more about the vaccinations you’ll be offered at school
If you have any questions on the day, you can speak to the person giving you the vaccine.
If you missed your vaccination and you’re still at school
If you miss your HPV vaccination, there will be further opportunities to get it. For example, you may be offered a rescheduled vaccination appointment next year.
If you’re unsure if you’ve missed any other vaccines, you should
first check your red book. If you do not have a red book, or it has gone missing, you can check with your local NHS immunisation team.
Young people not in mainstream education
You’re also eligible for the HPV vaccine if you’re:
- educated at home
- not in mainstream education
Please contact your local NHS immunisation team to arrange your appointment.
If your child is home schooled and has missed out on any vaccinations and you with them to be vaccinated. Then please ask your GP Practice to refer you to the Child Vaccination Team for this. On receipt of the referral the team will be in touch with you to arrange this.
If you’ve missed your vaccination and have now left school
If you’ve left school and you didn’t get your HPV vaccine when you were eligible, you may still be able to get it up until you turn 25.
This only applies to:
- people who are currently eligible
- boys who became eligible from the 2019/2020 academic year
- girls under 25 who were eligible under routine and catch up programmes introduced in 2008
Your local NHS immunisation team can confirm if you’re eligible. They can also explain how to get the HPV vaccine in your area.
If you / your child does not attend school or has missed vaccinations given in school, please contact the School Team listed under FAQs ‘School Team Contact Details’.
The vaccine consent form
You should be given a consent form and leaflet by your school. You and your parent or carer should chat about the information. Both you and your parent or carer should sign the consent form and return it to your school. You should return the consent form even if you’re not going to have the vaccine.
We recommend you get agreement from your parent or carer, but it isn’t always necessary.
MMR Vaccine – S1 – S6
The MMR vaccine is given in 2 doses and helps protect against measles, mumps and rubella. Find out more about the vaccine, and when and where to get it.
Why should someone have the MMR vaccination?
The MMR vaccine helps to protect people against measles, mumps and rubella. It’s sometimes also offered to adults who missed their childhood immunisations.
Measles, mumps and rubella are highly infectious diseases. They can cause serious medical complications.
A high number of people in Scotland have had the MMR vaccine. This means there’s been a big reduction in the number of people catching these diseases.
Who is eligible for the MMR vaccine?
All babies and children in Scotland are eligible for the MMR vaccine.
They’ll be offered the MMR vaccine in 2 doses:
- the first between 12 and 13 months
- the second at 3 years 4 months
Although normally given at these times, if it’s missed, it can be given at any age.
Some young people and adults who missed out on their MMR vaccine may also be eligible, like those who are a planning a pregnancy. If you didn’t have 2 doses of the MMR vaccine as a child, you can contact your local NHS immunisation team to discuss your eligibility.
If you / your child does not attend school or has missed vaccinations given in school, please contact the School Team listed under FAQs ‘School Team Contact Details’.
If your child is home schooled and has missed out on any vaccinations and you with them to be vaccinated. Then please ask your GP Practice to refer you to the Child Vaccination Team for this. On receipt of the referral the team will be in touch with you to arrange this.
DTP Vaccine – S3 to S6
The DTP vaccine provides protection against diphtheria, tetanus and polio. The vaccine is usually given in S3 (around 14 years old). Find out when and where to get it.
What the DTP vaccine is for
Immunisation (vaccination) information in other languages and formats
The DTP vaccine protects against diphtheria, tetanus and polio. These are serious diseases.
You need a total of 5 doses of the diphtheria, tetanus and polio vaccine to build up immunity and give you longer-term protection.
You should have had:
- the first 3 doses as a baby
- the fourth dose before you started primary school (after turning 3 years and 4 months)
You should have the fifth dose in S3 (around 14 years old).
What’s diphtheria?
Diphtheria is a serious disease that usually begins with a sore throat. It can quickly cause breathing problems. It can also damage the heart and nervous system, and in severe cases, can kill. Diphtheria is passed from person to person through close contact.
Before the diphtheria vaccine was introduced in the UK, there were up to 70,000 cases of diphtheria a year. These caused around 5,000 deaths.
What’s tetanus?
Tetanus is a painful disease affecting the nervous system that can lead to:
- muscle spasms
- breathing problems
- death
It’s caused by germs found in soil and manure getting into the body through open cuts or burns.
Tetanus can’t be passed from person to person.
What’s polio?
Polio is a virus that attacks the nervous system and can cause permanent paralysis of muscles. If it affects the chest muscles or the brain, polio can kill. The polio virus is usually spread from person to person or by swallowing contaminated food or water.
Before the polio vaccine was introduced, there were as many as 8,000 cases in the UK during the polio epidemic.
Who can get the DTP vaccine
All young people in S3 (around 14 years old) are eligible for the vaccination. This is part of their routine immunisation schedule.
- If you were immunised as a child – The DTP vaccine completes the 5 dose course against diphtheria, tetanus and polio. Although you’ve already had 4 doses of diphtheria, tetanus and polio vaccines, , you need a total of 5 to build up your immunity and provide longer-term protection.
- Reasons you should not have the vaccine – here are very few young people who can’t have the DTP vaccine. You shouldn’t have the vaccine if you’ve had a confirmed anaphylactic reaction to:
- a previous vaccine
- any ingredient of the vaccine
- neomycin, streptomycin or polymyxin B (antibiotics that may be added to vaccines in very tiny amounts)
- If you have a bleeding disorder – If you have a bleeding disorder, tell the person giving you the vaccine. They’ll give the injection in a slightly different way that will be better for you.
About the DTP vaccine
The REVAXIS vaccine is routinely used in Scotland.
The DTP vaccine is not a live vaccine. It cannot cause the diseases it protects against.
The DTP vaccine is the safest and most effective way to protect against serious diseases.
How to get the DTP vaccine
You’ll be offered the DTP vaccine when you’re in S3 (around 14 years of age) at school. Vaccines are given by your local NHS immunisation team. Your school will tell you when vaccination sessions are taking place.
Find out more about the vaccinations you’ll be offered at school
If you have any questions on the day, you can speak to the person giving you the vaccine.
If you / your child does not attend school or has missed vaccinations given in school, please contact the School Team listed under FAQs ‘School Team Contact Details’.
If your child is home schooled and has missed out on any vaccinations and you with them to be vaccinated. Then please ask your GP Practice to refer you to the Child Vaccination Team for this. On receipt of the referral the team will be in touch with you to arrange this.
Meningitis ACWY (MenACWY) vaccine – S3 to S6
The meningitis ACWY (MenACWY) vaccine helps protect against meningitis and septicaemia (blood poisoning). Find out more about the MenACWY vaccine, and when and where to get it.
What the Meningitis ACWY (MenACWY) vaccine is for
Immunisation (vaccination) information in other languages and formats
The meningitis ACWY (MenACWY) vaccine helps protect against meningitis and septicaemia (blood poisoning), which are caused by meningococcal bacteria A, C, W and Y.
Young people have a higher risk of getting meningococcal disease. You’ll be offered immunisation to protect yourself and others around you.
Meningitis and septicaemia are very serious diseases. They can cause permanent disability and death. The symptoms can come on quickly.
Who can get the MenACWY vaccine
The MenACWY vaccine is routinely offered to all young people in S3 (around 14 years of age). If you’re over 14 and not already immunised, you may also be offered the vaccine.
You should not have some vaccines if you’ve had a confirmed anaphylactic shock (serious allergic reaction) to:
- a previous vaccine
- any ingredient of this vaccine
About the MenACWY vaccine
The following vaccines are routinely used in Scotland:
- Menveo Meningococcal Group A, C, W135 and Y conjugate vaccine
- Nimenrix powder and solvent for solution for injection in pre-filled syringe
The MenACWY vaccine is highly effective at protecting against the serious infections caused by meningococcal bacteria A, C, W and Y.
The MenACWY vaccine is not a live vaccine. It cannot cause meningitis.
The MenACWY vaccine is the safest and most effective way to protect against meningococcal A, C, W and Y.
How to get the MenACWY vaccine
Vaccines are given by your local NHS immunisation team. Your school will tell you when vaccination sessions are taking place.
Find out more about the vaccinations you’ll be offered at school
If you have any questions on the day, you can speak to the person giving you the vaccine.
If you missed your vaccination at school
If you missed your MenACWY vaccination, there will be further opportunities to get it. For example, you may be offered a rescheduled vaccination appointment next year.
If you’re unsure if you’ve missed any other vaccines, you should first check your red book. If you do not have a red book, or it has gone missing, you can check with your local NHS immunisation team
Young people not in mainstream education
You’re also eligible for the MenACWY vaccine if you’re:
- educated at home
- not in mainstream education
If you / your child does not attend school or has missed vaccinations given in school, please contact the School Team listed under FAQs ‘School Team Contact Details’.
If your child is home schooled and has missed out on any vaccinations and you with them to be vaccinated. Then please ask your GP Practice to refer you to the Child Vaccination Team for this. On receipt of the referral the team will be in touch with you to arrange this.
Students
You may be eligible for the MenACWY vaccination if you:
- are Scottish and attending further education in Scotland
- are aged up to 25 years old
- have not had the MenACWY vaccination
You should contact your local NHS immunisation team. They’ll advise you if it’s clinically appropriate for you to have the vaccine.
You may not be eligible for the MenACWY vaccination if you’re from outside Scotland (including other parts of the UK). You should arrange to get your vaccine before travelling to Scotland. There’s no guarantee the vaccine will be available to you after arriving in Scotland.
Seasonal Vaccination
Pre-School 6 Months to 2 Years at Risk – Flu
NHS Scotland recommends eligible children should get the flu vaccine to help protect them from influenza (flu).
Flu (influenza) is a common infectious respiratory virus. Symptoms may include a fever, a cough, a headache, and tiredness.
Why should I have my child vaccinated?
Flu can be serious. Even healthy children can become seriously ill from flu. In some cases flu can lead to complications. These can include bronchitis, pneumonia, painful middle-ear infection, vomiting, diarrhoea. In the worst cases, flu can lead to disability and even death.
Flu can be even more serious for people with health conditions such as:
- asthma
- heart, kidney, liver or neurological disease
- diabetes
- a weakened immune system
- a spleen that does not work fully
Flu can make health conditions worse.
The flu vaccine will reduce the risk of your child getting or spreading flu to friends and family who are at greater risk from flu. For example, grandparents or people with health conditions. It’ll also help prevent your child getting sick with flu and needing time off school or nursery.
How is the vaccine given?
Children aged 6 months to 2 years will be given the injectable flu vaccine.
Vaccine safety
All medicines, including vaccines, are tested for safety and effectiveness before they’re allowed to be used.
Once they’re in use, the safety of vaccines continues to be monitored by the Medicines and Healthcare products Regulatory Agency (MHRA).
The nasal spray flu vaccine has been used since 2014 and has a good safety record. Millions of doses of the vaccine have been given to children in the UK.
Does the vaccine work?
The annual vaccine offers protection against the most common types of flu virus that are around each winter. The flu vaccine should start to protect most children about 10 to 14 days after they receive their vaccination.
In previous years, the flu vaccine has worked very well, providing protection against flu. It has also reduced the chance of spreading flu into the wider community.
Pre-School 6 Months to 4 Years at Risk – Covid
NHS Scotland is offering the coronavirus (COVID-19) vaccine to children aged 6 months to 11 years at higher risk of coronavirus this spring.
To be invited for vaccination this spring, your child must have a weakened immune system and be aged 6 months to 11 years on 31 March 2024 (born on or after 1 April 2012 and before 1 October 2023).
Why is my child being offered the coronavirus vaccine?
Getting the vaccine will help to protect your child against coronavirus. The vaccine helps to build up immunity to coronavirus, so the body can fight it off more easily. If your child is vaccinated, they are much less likely to get seriously ill from coronavirus or need to go to hospital.
Infants and young children with underlying health conditions are 7 times more likely to be admitted to paediatric intensive care units with severe coronavirus, compared to those without underlying health conditions.
My child has already had the coronavirus vaccine – do they need another one?
NHS Scotland is offering a coronavirus vaccine to children at higher risk to help protect them this spring. It’s important to keep up to date with the coronavirus vaccines your child is offered.
NHS Scotland recommends coming forward every time your child is invited to keep their protection topped up.
Is the coronavirus vaccine safe?
NHS Scotland will only use a vaccine if it meets the required standards of safety and effectiveness. All medicines, including vaccines, are tested for safety and effectiveness before they’re allowed to be used. The Medicines and Healthcare products Regulatory Agency (MHRA) assesses all the data and also ensures a vaccine works and that all the necessary trials and checks have been completed.
Are there any reasons my child should not get the coronavirus vaccine?
There are very few people who cannot have the vaccine. If your child has had a confirmed severe allergic reaction (anaphylaxis) to any of the vaccine ingredients or a previous dose of the same vaccine, you should seek advice from your health professional before your child has the vaccine.
The vaccine is not a live vaccine and does not contain any animal products or egg.
Vaccine manufacturer patient information leaflets
More information about the vaccines offered, including vaccine ingredients, is available in the manufacturer patient information leaflets.
Read the coronavirus vaccine patient information leaflet for 6 months to 4 years:
Pre-School 2 – 5 year old childhood flu
NHS Scotland recommends eligible children should get the flu vaccine to help protect them from influenza (flu).
The flu vaccine is available between September and March.
Flu (influenza) is a common infectious respiratory virus. Symptoms may include a fever, a cough, a headache, and tiredness.
The flu vaccine is offered as a painless nasal spray to almost all children. It cannot give the child flu but starts to provide protection against flu within 10-14 days. The nasal spray offers the best possible protection for children and young people and can also stop flu spreading to family, friends and others, especially those most at risk of becoming seriously ill with flu. Children aged 2 to 5 are being offered vaccination from the start of the programme to ensure they receive the earliest protection and prevent the virus spreading.
Why should I have my child vaccinated?
Flu can be serious. Even healthy children can become seriously ill from flu. In some cases flu can lead to complications. These can include bronchitis, pneumonia, painful middle-ear infection, vomiting, diarrhoea. In the worst cases, flu can lead to disability and even death.
Flu can be even more serious for people with health conditions such as:
- asthma
- heart, kidney, liver or neurological disease
- diabetes
- a weakened immune system
- a spleen that does not work fully
Flu can make health conditions worse.
The flu vaccine will reduce the risk of your child getting or spreading flu to friends and family who are at greater risk from flu. For example, grandparents or people with health conditions. It’ll also help prevent your child getting sick with flu and needing time off school or nursery.
How is the vaccine given?
In Scotland, children aged 2 to 17 will usually be given the nasal spray flu vaccine. It’s quick and painless and there’s no need to sniff or inhale the vaccine. It’ll just feel like a tickle in their nose.
Children aged 2 to 17 years who cannot receive the nasal spray vaccine will receive the injectable flu vaccine.
Vaccine safety
All medicines, including vaccines, are tested for safety and effectiveness before they’re allowed to be used.
Once they’re in use, the safety of vaccines continues to be monitored by the Medicines and Healthcare products Regulatory Agency (MHRA).
The nasal spray flu vaccine has been used since 2014 and has a good safety record. Millions of doses of the vaccine have been given to children in the UK.
Does the vaccine work?
The annual vaccine offers protection against the most common types of flu virus that are around each winter. The flu vaccine should start to protect most children about 10 to 14 days after they receive their vaccination.
In previous years, the flu vaccine has worked very well, providing protection against flu. It has also reduced the chance of spreading flu into the wider community.
Primary School Children – Flu
NHS Scotland recommends eligible children should get the flu vaccine to help protect them from influenza (flu).
The flu vaccine is available between September and March.
Flu (influenza) is a common infectious respiratory virus. Symptoms may include a fever, a cough, a headache, and tiredness.
The flu vaccine is offered as a painless nasal spray to almost all children. It cannot give the child flu but starts to provide protection against flu within 10-14 days. The nasal spray offers the best possible protection for children and young people and can also stop flu spreading to family, friends and others, especially those most at risk of becoming seriously ill with flu.
Consent forms and further information will be sent home to parents and carers of school children on return to school. Secondary pupils can self-consent but are encouraged to speak to a parent or carer first. All primary and secondary school pupils with consent to be given the flu vaccine nasal spray will receive this at school starting in early September through to December 2024.
Why should I have my child vaccinated?
Flu can be serious. Even healthy children can become seriously ill from flu. In some cases flu can lead to complications. These can include bronchitis, pneumonia, painful middle-ear infection, vomiting, diarrhoea. In the worst cases, flu can lead to disability and even death.
Flu can be even more serious for people with health conditions such as:
- asthma
- heart, kidney, liver or neurological disease
- diabetes
- a weakened immune system
- a spleen that does not work fully
Flu can make health conditions worse.
The flu vaccine will reduce the risk of your child getting or spreading flu to friends and family who are at greater risk from flu. For example, grandparents or people with health conditions. It’ll also help prevent your child getting sick with flu and needing time off school or nursery.
How is the vaccine given?
In Scotland, children aged 2 to 17 will usually be given the nasal spray flu vaccine. It’s quick and painless and there’s no need to sniff or inhale the vaccine. It’ll just feel like a tickle in their nose.
Children aged 2 to 17 years who cannot receive the nasal spray vaccine will receive the injectable flu vaccine.
Children aged 6 months to 2 years will be given the injectable flu vaccine.
Vaccine safety
All medicines, including vaccines, are tested for safety and effectiveness before they’re allowed to be used.
Once they’re in use, the safety of vaccines continues to be monitored by the Medicines and Healthcare products Regulatory Agency (MHRA).
The nasal spray flu vaccine has been used since 2014 and has a good safety record. Millions of doses of the vaccine have been given to children in the UK.
Does the vaccine work?
The annual vaccine offers protection against the most common types of flu virus that are around each winter. The flu vaccine should start to protect most children about 10 to 14 days after they receive their vaccination.
In previous years, the flu vaccine has worked very well, providing protection against flu. It has also reduced the chance of spreading flu into the wider community.
Where clinics take place
Vaccinations are typically given in schools during term time. NHS GGC work with schools to communicate programme dates.
Before clinics take place, consent forms and vaccination information will be handed out to pupils at school for review at home then return to school.
If you / your child does not attend school or has missed vaccinations given in school, please contact the School Team listed under FAQs ‘School Team Contact Details’.
On the day
Pupils will usually attend clinics in the school hall or social space, class by class throughout the day.
Secondary School Children and Young People – Flu
About the programme
Immunisation is the safest and most effective way of protecting young people against serious diseases.
School-aged children are routinely vaccinated against:
- Influenza – usually offered to all primary and secondary school pupils from September to December .
The flu vaccine is offered as a painless nasal spray to almost all children. It cannot give the child flu but starts to provide protection against flu within 10-14 days. The nasal spray offers the best possible protection for children and young people and can also stop flu spreading to family, friends and others, especially those most at risk of becoming seriously ill with flu.
Consent forms and further information will be sent home to parents and carers of school children on return to school. Secondary pupils can self-consent but are encouraged to speak to a parent or carer first. All primary and secondary school pupils with consent to be given the flu vaccine nasal spray will receive this at school starting in early September through to December 2024.
https://www.nhsinform.scot/vaccineconsentyoungpeople
For details of the schedule of vaccinations in Scotland by age, please refer to NHS Inform.
Where clinics take place
Vaccinations are typically given in schools during term time. NHS GGC work with schools to communicate programme dates.
Before clinics take place, consent forms and vaccination information will be handed out to pupils at school for review at home then return to school.
If you / your child does not attend school or has missed vaccinations given in school, please contact the School Team listed under FAQs ‘School Team Contact Details’.
On the day
Pupils will usually attend clinics in the school hall or social space, class by class throughout the day.
FAQs
I am unsure of my child’s immunisation history
Please contact your GP
Pre-School Team Contact Details
Please see team contact details below:
Glasgow South/East Renfrewshire
Phone Number: 0141 577 7774 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
Health Centres: Castlemilk, Eastwood, Govanhill, Gorbals, Govanhill (EU), Pollock, Shields Centre, Elderpark, Thornliebank, Barrhead
North East/East Dunbartonshire
Phone Number: 0141 531 6635 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
Health Centres: Springburn, Kirkintilloch, Stobhill, Milngavie, Baillieston, Shettleston, Bridgeton, Townhead, Easterhouse
North West/West Dunbartonshire
Phone Number: 0141 211 6142 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
Health Centres: Dumbarton, Vale of Leven, Maryhill, Woodside, Possilpark, Community Centre for Health (CCFH), Plean Street, Drumchapel, Clydebank
Renfrewshire/Inverclyde
Phone Number: 0141 201 1056 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
Health Centres: Greenock, Port Glasgow, Johnstone, Linwood, Renfrew, Foxbar Clinic, Northcroft, Tannahill Centre, Erskine
School Team Contact Details
Please see team contact details below:
Glasgow South/East Renfrewshire
Phone Number: 0141 577 7767 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
North East/East Dunbartonshire
Phone Number: 0141 232 9838 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
North West/West Dunbartonshire
Phone Number: 0141 232 9202 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
Renfrewshire/Inverclyde
Phone Number: 0141 314 0513 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
Was this helpful?
When you or someone you care about becomes ill, life can become very stressful. That is why we think it is so important for people to talk to each other and make plans before this happens.
To help people plan more, and stress less, we have created a toolkit of resources that we hope will be useful. This includes the recorded information session below and checklists to help you get organised, as well as a plan to work out how you’d get home from hospital. We also look at some of the legal process and support that is available for those who care for you.
Even if you and those you support are perfectly healthy just now, you can still use these tools to help plan for the future!
We have recorded the “Plan More, Stress Less” session below for anyone interested in getting started with planning ahead. In this session we talk about what paperwork we can complete before a crisis arises, what actually happens when someone goes into hospital and how we can all work together to plan for a safe and timely discharge.
Watch the recording here:
Alongside this video we have created two resources which anyone can use to help them plan for any future hospital admission. This could be a planned admission, for example if someone is going to hospital for an operation or to have some tests. However these resources can also be useful if someone needs to go to hospital in an emergency.
If you have any questions or feedback about these resources please email ggc.HomeFirst@nhs.scot
Preparing for Hospital Checklist
This checklist will help you think about all the different forms which you can complete just now that would be useful if you were ever in hospital. This includes things like a Future Care Plan and a Power of Attorney.
A Plan to Get You Home
This resources lets you and the people who support you, think about what might need to happen in order to get you home from hospital in a safe and timely manner. This includes thinking about who could collect you from hospital and where you might need to live if you need some extra support for a short time or on a more permanent basis.