A woman whose lung cancer was detected with the help of Artificial Intelligence has praised the “incredible” speed of her diagnosis and treatment.
Diane McCallum, 60, was referred for a chest X-ray at New Stobhill Hospital by her GP in April this year after she had been struggling with a long-term, persistent cough.
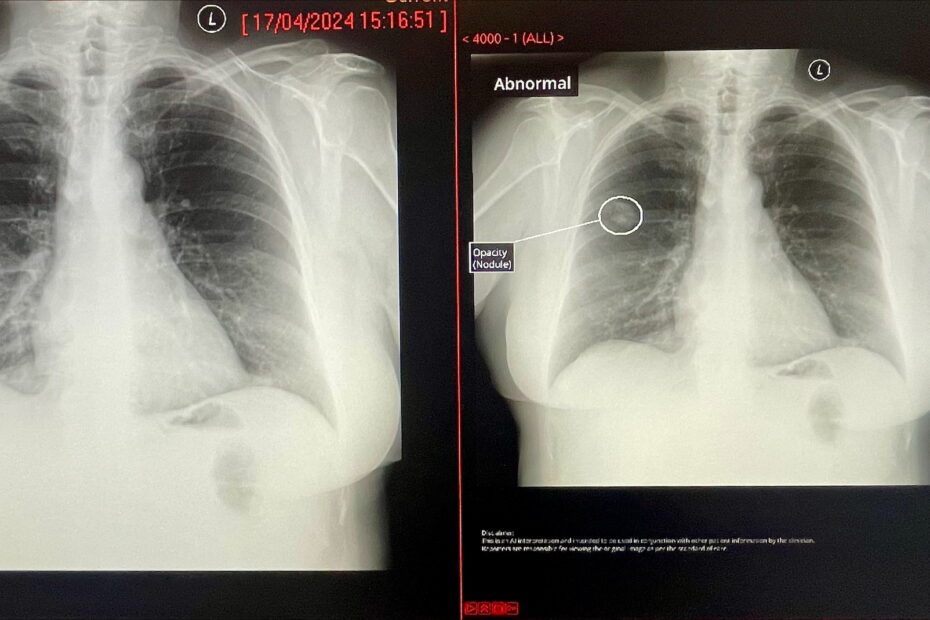
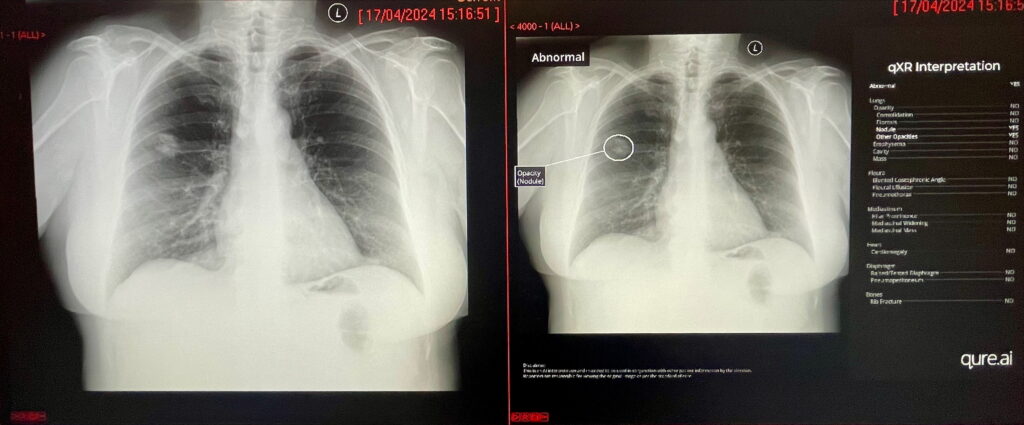
Her X-ray image was analysed by AI software, qXR, which flagged up an abnormality and placed it in a priority pile for examination by a radiologist.
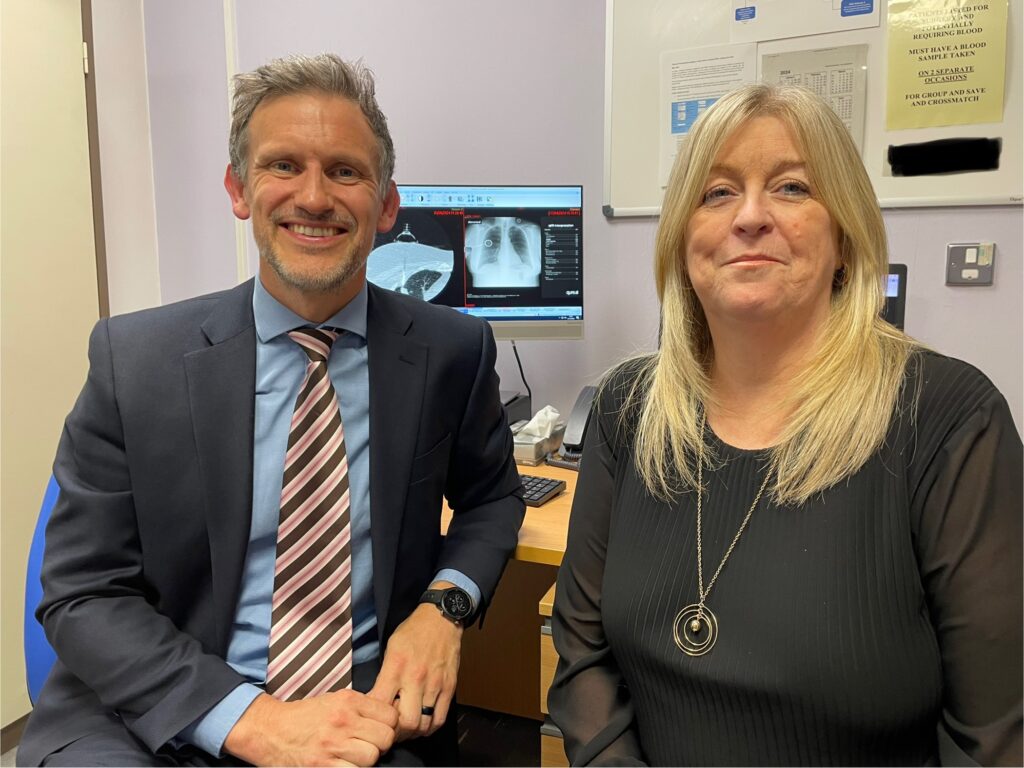
Within hours, Diane had been contacted and referred for a CT scan which helped confirm her diagnosis of early-stage lung cancer, and treatment was arranged by NHS Greater Glasgow and Clyde Respiratory Consultant Dr John MacLay.
She was operated on using robotic keyhole surgery at the Golden Jubilee Hospital to remove the upper lobe of her right lung.
The mum-of-three, who has one young grandchild, is now in the process of having four rounds of preventive chemotherapy at the Beatson West of Scotland Cancer Centre to reduce the chance of any cancer returning.
In total, her diagnosis and delivery of treatment took around seven weeks, with AI being used to “fast track” her X-ray image for the attention of clinicians rather than it being sifted through along with hundreds of “normal” images.
qXR is being used as part of a clinical study and has been deployed as a collaboration between innovator Qure.ai, the NHSGGC-hosted West of Scotland Innovation Hub, the University of Glasgow and the Chief Scientist Office of the Scottish Government.
It is also supported by NHSGGC’s Diagnostics Directorate and Digital Services.
The RADICAL (Radiograph Accelerated Detection and Identification of Cancer of the Lung) trial has been underway across NHSGGC for the past year, with AI used to analyse chest X-rays in near real-time.
The Qure.ai solution automatically segregates ‘normal’ chest X-rays and flags abnormalities such as masses or lung nodules, enabling the prioritisation of patient case reporting for clinicians – speeding up the start of a patient’s care journey from weeks to days.
The software is being used in all outpatient chest X-rays, for example, in those who fall and break a rib and where there is no suspicion of cancer.
This means members of the population are being screened for lung cancer even when there is no suspicion of it, and could potentially result in problems being identified at a much earlier stage than may have otherwise been the case.
Lung cancer remains the most common cause of death from cancer in Scotland. It is also the most common cancer overall, with 5,476 cases diagnosed in 2021, accounting for 15.5% of all cancers in Scotland.
Diane, an NHS worker from Bishopbriggs, near Glasgow, shared her story as NHSGGC marks Lung Cancer Awareness Month during November.
She told how the speed of her diagnosis and treatment helped alleviate some of the anxiety she and her family were feeling when she first found out she had cancer.
Diane said: “When I went for my X-ray in May I remember seeing a poster in the hospital explaining the trial using AI and even at that point I was really impressed.
“I had my X-ray at about 3.30pm, and by 9.15am the following day I’d had a phone call to say something had been found and that I was being referred for CT imaging.
“After that, everything moved so quickly and my Consultant Dr MacLay said the cancer was quite early and localised, and he told me they were going to throw everything at it.
“I then had the operation to remove my right upper lobe using robotic keyhole surgery, which was also very impressive and meant my recovery was good.
“Everything about it was incredible, but the best thing for me was that X-ray.
“It just meant everything from that point was dealt with so quickly. It made such a difference for it all to happen within weeks rather than months and meant the cancer wasn’t able to spread.
“My outcome is undoubtedly better than if it has been left there to get worse.
“Having the AI enhancement at the beginning of the process is life saving really. Who knows how it might have turned out without this AI.”
The qXR AI solution is being supported by the University of Glasgow’s Digital Health Validation Lab, part of the Living Laboratory for Precision Medicine, providing leadership to deliver the trial alongside NHSGGC and Qure.ai.
By diagnosing lung cancer earlier, at stage 2, more than 40% of patients will survive their cancer for longer than five years. This rises to more than 65% if diagnosed at stage 1. This is in stark contrast to less than 5% five-year survival at late-stage 4 diagnosis.
Professor David Lowe, Professor of Health Innovation at the University of Glasgow and Emergency Medicine Consultant at NHS Greater Glasgow and Clyde, said: “Worldwide healthcare systems have a significant challenge in the detection of lung cancer.
“At present, 40-50% of patients present with advanced or stage 4 cancer, leading to poorer outcomes.
“If we can spot cancer earlier, by speeding up the time and accuracy of the 100,000 chest X-rays performed each year at NHSGGC, we can improve time to further imaging, and subsequent treatment.
“Qure’s chest X-ray AI, which is being evaluated as part of the RADICAL study across NHSGGC, will help orchestrate benefits for the whole patient care pathway.”
Respiratory Consultant Dr John MacLay said: “If you turn up for an X-ray in the traditional way, the report goes into one pile.
“With this AI software, it reads the X-ray quickly – almost immediately – and sorts the X-ray reports into two piles: a priority pile for patients where an abnormality has been detected in their X-ray, and one that is not quite as high a priority as no abnormalities have been found.
“That allows radiologists to triage these and hopefully as part of the study we will be able to show that this enables us to get these patients through to CT scans quicker, and to have a diagnosis of lung cancer quicker.
“We know that the quicker we get to the diagnosis of lung cancer the quicker we can manage it, and the less likely patients are to become incurable.
“Diane attended for an X-ray and her results would have gone into the fast reporting queue because of the abnormality it flagged.
“Within a few days she had a CT scan and came to see a respiratory physician, and then was treated for lung cancer with surgery in a matter of weeks – when often that pathway can run into months.
“It also meant her stage of lung cancer didn’t migrate into a more significant stage that would become more difficult to treat.”
Shamie Kumar, Senior Director and Clinical Specialist at Qure.ai, said:
“qXR is an AI software that has been deployed in more than 50 countries globally and it is used in multiple NHS sites around the UK.
“It is trained to pick up over 30 abnormalities in chest X-rays, triaging and prioritising the most important patient cases for radiologists to look at first.
“Chest X-rays happen in large volumes within hospitals and this software will detect, segregate and label what it has found.
“Diane’s story is quite amazing – we are delighted to hear her real-life experience of how the qXR AI technology has been part of her diagnostic journey. At the heart of all our AI innovations is a patient. We hope that the activation of AI into healthcare continues at pace to positively impact people on a larger scale in the fight against lung cancer.”
Dr Katriona Brooksbank, R&I Innovation Lead for West of Scotland Innovation Hub, hosted by NHSGGC, said: “We are the sponsor of the ethically-approved RADICAL research study and the Hub is project managing its delivery.
“This is an absolutely great example of where AI can add value in healthcare.
“The study allows us to look for early signs of lung cancer in everybody who attends for an outpatient chest X-ray.
“The West of Scotland Innovation Hub is looking at a broad strategy of safely assessing the added value of AI tools in a range of clinical pathways including like RADICAL in real-time workflow prioritisation.
“This means we don’t replace human clinician interaction with patients with technology, but we use the technology to look quicker and faster at the data presented to them and allow clinicians to be directed to where their expertise is required for the human elements of the care the NHS can give.
“Diane’s case is a brilliant example of why we do what we do.”
Neil Warbrick, NHSGGC’s Head of Strategy, Programmes and Innovation, said: “AI is ready for adoption into clinical practice within this area of national priority. Products such as qXR from Qure.ai will help us to detect lung cancer early, this project will establish reliable evidence of impact and value, and under our Digital Strategy’s ‘Enabled by AI Programme’ is part of our ongoing work in NHS Greater Glasgow and Clyde to co-develop and adopt digital solutions that support clinical decision making.”