The approach to dealing with mental ill-health has been transformed in the last 70 years. The old asylums have been closed and most care is now within the community. However, if someone does need treatment in an acute ward, then some of the old stigma – and fear – surrounding going into hospital remains. But teams at Glasgow’s Leverndale Hospital have been working hard to transform what people can expect when they need the most support.
“You’re not going to stay here forever, that’s not the business we’re in,” explained Jennifer Wyld, Senior Patient Activity Co-ordinator Nurse at the hospital. On average, she says, most people stay in hospital for less than one month.
She added: “If you’re being admitted to any mental health hospital, it must be terrifying. If you are being admitted, you are probably quite unwell and experiencing symptoms that are very confusing and distressing.
“We start by dealing with people calmly and compassionately, and help them to start to feel assured that they are in a place of safety where people understand them. I can make a promise to people that they will get better and they will go home.”
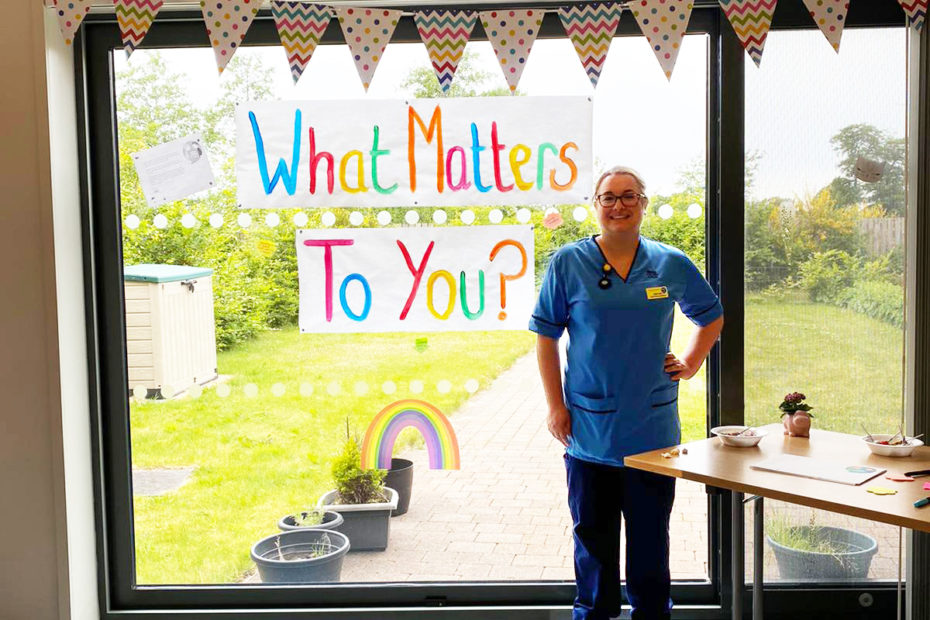
As well as providing specialist care, Jennifer and the team work to provide activities that stimulate, with everything from psychological therapies, to football groups, art therapy sessions and welfare rights sessions. The 1970s wards and surrounding areas have been transformed to provide colour and life.
Jennifer added: “Gone are the days where you just rely on medication and people are sent to an institution where they just languish.
“What we hear from patients is them saying. ‘oh I never expected it be like this, it’s so normal.’ It’s about making a difference and it can be the smallest things – sometimes it’s just about offering a cup of tea and taking two minutes to go for a walk that helps someone feel better.
“I’ve got the best job in the hospital, I help people to flourish.”
COVID has meant some changes to the help on offer, blending support with classes and technology, building skills which reduce isolation and open new doors.
Samantha Flower, is an Occupational Therapy Mental Health Advisor and has led on improving the greenspace around the hospital. Working with an artist, they involved the service users, carers and staff to design and create works which are woven into the natural spaces with service users’ designs included in the mosaic tiles installed on site. She said: “I’ve worked with people who have significant mental health issues, but are really fantastic artists, or horticulture therapists, creative writers and photographers who have gone on to make a living out of this.
“It’s about maximising potential – it doesn’t matter if you have mental health diagnosis you can still lead a fulfilling life. Just because you’ve been hospitalised doesn’t mean you can’t get better and thrive.”
The outdoor space has been transformed into a blossoming landscape, where the hospital community and nature can thrive, with improved wayfinding, art interventions and even a service user inspired mural.
“You can do one little thing and it lights people’s imaginations,” added Samantha. “This is a hospital, a place of safety – there is life here, creativity and joy.”