Meeting the needs of BME people
This information is for the attention of all NHSGGC staff involved in the treatment and care of Black and Minority Ethnic patients (BME). Following these guidelines will help ensure that our BME patients access the services and treatments that meet their needs. This information is also available on the Right Decisions app.
Around 5% of our BME patients do not speak English. This group of patients have additional barriers to accessing our services that must be addressed.
Getting It Right for BME patients – Core Elements
Expectations for all NHSGGC staff
Treat people fairly – treat BME people fairly and without prejudice or stereotyping. NHSGGC has a zero tolerance policy on discrimination.
Know your community – have knowledge of the local community who may use their service, including an ethnicity and language breakdown.
Collect ethnicity data – always collect the ethnicity of patients using your service. This is mandatory in Scotland for Acute services. TrakCare care and EMIS enable you to record the ethnicity of people who use our services in the demographics pages. People can say ‘prefer not to say’ but we need to ask all people who use our services. Anyone who comes into contact with a patient and has responsibility for checking their demographics to confirm identification and should update their details including ethnicity. Patient demographics which includes ethnicity should be checked on every visit for every patient to a hospital to ensure it is fully updated. If available on paperwork prior to visit e.g. through a GP Referral, then whomever is logging this on the system should update demographics. The patient does not always need to be present for the first update. All patient must have their ethnicity recorded.
Prepare translated resources – have resources about your service ready, including consent to treatment forms, for your BME patients who may not speak English. Have a stock available in the languages you use most and know how to access others when required. For more information go to Clear to All.
Know how to access interpreting support – It is our responsibility to provide interpreting support for any patients using our services. Support is available either via telephone or face to face interpreters. For more information go to Interpreting Services
Ensure patients know how to access interpreting support – patients who don’t speak English can use our telephone interpreting service to call your or any other NHSGGC service. Patient leaflets are available for immediate download in 40 languages. See Direct Patient Access information. Other languages can be provided for your patient.
Get feedback from BME patients – ensure that any patient engagement is inclusive of BME communities, including non-English speakers
Know how to access staff training that covers race equality – you can log in to LearnPro for the statutory and mandatory equality training
Source: Joseph Rowntree Foundation
Know your population
Scotland’s BME population
The 2022 Census has provided evidence of the changing ethnic composition of Scotland.
Of the 5.4 million people living in Scotland, around 388,000 came from Black/Minority Ethnic backgrounds, which equates to around 7% of the total population – a rise of 3% from the 2011 census figures.
Asian groups were the largest minority ethnic group in Scotland and represent nearly 4% of the total population. White minority ethnic groups (e.g. Irish, Gypsy/Traveller, Polish) collectively make up 5.8% of the total population – a rise of 1.6% since the 2011 census.
Scotland’s BME population is patterned by age, with 11.6% of Scotland’s total population being BME people under the age of 18. This compares to just 1.5% of Scotland’s total population being BME people over the age of 65.
Glasgow is the most ethnically diverse place in Scotland with 20% of Glaswegians coming from BME backgrounds. Notably 32.6% of Glasgow’s under 18 year olds come from BME backgrounds.
Community Languages
About 5 in every 100 people admitted to our hospitals as inpatients do not speak English.
NHSGGC has over 100 language groups that use our services. The top 10 languages are currently:
- Arabic
- Urdu
- Polish
- Mandarin
- Romanian
- Farsi
- Punjabi
- Kurdish Sorani
- Cantonese
- Slovakian
Your service’s patient population may not reflect these main language groups so it is important to monitor this. For example, a patient population which is mainly drawn from refugees and asylum seekers will have a different language profile.
Engagement
Services need to establish an understanding of needs by engaging with BME patients and staff to identify issues for BME patients in our services. This can include data collection around ethnicity. It is important to note that all of us have an ethnicity and therefore all patients should be asked their ethnicity in our services.
Services should regularly engage with patients to understand what they think about the services we provide. It is important to include BME patient specifically in patient engagement to ensure their voice is heard in how to improve services. Speak to the Board’s Patient Experience and Public Involvement Team (PEPI) for advice.
Taking an anti-racist approach
Taking an anti-racist approach means ensuring that how we behave or design and operate our services does not discriminate against BME people.
Discrimination means treating people less favourably due to their colour, nationality (including citizenship), ethnicity or national origin (Equality Act (2010)). We all have an ethnicity.
As NHSGGC staff we need to recognise that racism – or any form of discrimination – is a fundamental cause of poor health in affected populations.
We need to create an environment free from racism and stereotyping. We have a responsibility to deliver Person and Family Centred Care to all our patients, based on their individual needs and best practice. Do not make assumptions about a patient’s needs – ask them.
It’s important to recognise that being in the majority group brings with it a level of power and belonging that BME people may not attain. Pointing out perceived differences in appearance, describing BME patients as ‘not our patients’ or as ‘foreign’ when they were born here, all contribute to ‘othering.’
This ‘othering’ can often take the form of using offensive language. Sometimes people will describe certain language as ‘banter’ or ‘having a laugh,’ which can make it difficult for someone to challenge. It is important to always speak up and address the use of offensive language that may be heard in our services.
Racism is classed as a Hate Incident or Hate Crime and should be reported through the NHSGGC Datix Incident reporting system
Inclusive Care
Patient Information
Provision of patient information is a key aspect of health services whether this is written, verbal or in other formats.
Services should assess all patient facing written information to ensure it is accessible.
Identify the core information patients will need and have this available in plain English before requesting translations through the Clear to All service. Clinical letters, diagnostic instructions and compliance-related written information specific to an individual patient can also be translated through this service.
Some patients will wish to take home information about their condition in English, as well as the language they read. This is so family members who read only English are aware of the details.
If your service has high numbers of service users who do not speak English, identify the language profile over a few months and decide on an appropriate stock of your core service information in community languages. For example, in the NHSGGC area there are over 100 languages in use. Maternity Services reviewed their language profile and identified that their service information should be translated and made readily available in at least 10 community languages. Any language out with this list could then be requested via Clear to All as required.
Please be aware if your leaflet is providing additional information through links to English language websites. If the information is integral to the content, it should be translated and provided separately. Otherwise, the leaflet should include a statement to say, ‘If you are unable to access the information on this site, please speak to your clinician’.
All patient leaflets should include the NHSGGC statement regarding availability in accessible formats. For more information go to Alternative Format/Language text section at Interpreting & Language Resources.
When you have completed your review of your service leaflets and implemented this approach, ensure that all staff are aware of how and when to use patient information.
Consider, when making new resources, how this will be translated. This particularly relates to audio and video resources. Liaising with Clear to All is essential to establish the most suitable format. Videos can be voiced over (not subtitled) in community languages but ensure the images used in videos represent our diverse population.
Provision of Interpreting Support
It is our responsibility to provide interpreting support for any patients using our services. All staff should therefore have good awareness of and confidence in using the NHSGGC Interpreting Services.
Support is available either via telephone or face to face interpreters. For more information on how and when to use the service, and resources such as, How to Access Interpreting posters, go to Interpreting Services
Patients who don’t speak English can use our telephone interpreting service to call your or any other NHSGGC service. Please ensure that your patients are given an information leaflet explaining this service in the appropriate language. Leaflets are available for immediate download in 40 languages and can be requested if not currently available. See Direct Patient Access information.
If you or your service would like to attend training on how to use interpreting services, go to our training webpage.
Barriers to Accessing Services
Adopting a flexible appointments system will help ensure that non-English speaking patients have the time they need to communicate and understand any exchange. This also applies to anyone who needs additional time to speak or who uses communication support e.g. patients who have a learning disability, speech difference or British Sign Language user.
Cultural and social issues may be an additional barrier to accessing certain services for some BME communities. For example, there is not a specific word that means ‘depression’ in certain languages, including Punjabi, Urdu and Hindi. The stigma or lack of understanding of mental health problems may be a prohibiting factor for some individuals accessing any NHSGGC services. Also, if patients experience negative or racist attitudes from staff, this will prohibit them from engaging effectively with health services.
If there is a NHSGGC registered healthcare chaplain available on site, they can assist in supporting staff and BME patients and if appropriate, can access specific faith leaders that may provide reassurance for some BME patients. Visit our website for more information.
Community isolation may be a barrier for individuals from smaller BME groups or people who have sought asylum. These individuals may have little or no understanding of the availability of services or how they are provided. This can result in isolation from many statutory services, including the wider health services. Issues relating to migration status can exacerbate such problems.
Your service may work with particular voluntary organisations who could help with considering how best to reach and engage with BME communities. Organisations who can support staff include the Integration Networks e.g. Maryhill Integration Networks, Amma Birth Partners, Red Cross for asylum seekers and refugees.
Acute Patient Pathway – Issues to consider
Pre-admission/Admission
Where possible, ensure staff are aware of your patient’s additional support needs and condition history before they attend. SCI gateway referral letters should highlight if an interpreter is required and any other additional needs.
At times, however, this may not be listed on the referral letter.
It is good practice for staff to routinely ask, “Is there anything I need to be aware of when planning your care?” This may include barriers to accessing appointment times, preferred communication methods/support or issues with travel costs.
Ensure that the patient’s interpreter needs are recorded in the ‘demographics’ on TrakCare and not only on an alert. Update TrakCare if you have a patient who does not speak English and you were unaware of this before they attended their appointment.
Use telephone interpreting if a face to face interpreter was not secured, even to just re-appointment and explain what is happening. Telephone interpreting can be used for the majority of NHSGGC appointments.
Patients who require any kind of communication support will need flexibility within their appointment. Please provide this time to ensure that patients using an interpreter fully understand the information being conveyed and have the opportunity to ask any questions. Make sure that what you have said has been understood.
For face to face interpreting support, check if the patient has stated a preference for the interpreter’s sex.
Do not use family members or bilingual staff as interpreters. Do not use Google translate.
More information on NHSGGC’s policy regarding interpreting support can be found in the policy document.
During Stay
BME patients and carers should be supported and empowered to have their say regarding co-produced care and treatment plans.
Understanding the parameters of our services is important to all our patients. Staff should ensure that the patient understands the service or treatment and why they are receiving it to ensure compliance and consent. Checking that this information is fully understood will maximise benefits to the patient.
Do not exclude non-English speaking patients from group work – they should be offered every part of the patient pathway in line with English speaking patients. The Interpreting Service can offer interpreters who are particularly skilled at working in group settings and can advise staff accordingly.
Discharge
Check that your patient fully understands their discharge plan in terms of clinical follow-up, self-care and supports in the community. If interpreting support is required for this, note that this intervention will take a longer time to complete.
It is vital to use interpreting support at the point of dispensing medication to ensure your patient understands the purpose of their medications and when and how to take it.
Information prescriptions have been used to support this in some services, with translations made as required. Ensure your non-English speaking patient knows how to call back to the pharmacy if they have any questions about their medication, using the direct access telephone interpreting service.
BME communities in NHSGGC have high rates of poverty, and many patients can find themselves going home to difficult circumstances. Please use the Money Worries web page to access simple NHSGGC referral pathways to money advice services and interventions such as the Home Energy Crisis Response Service.
Supporting Information
Clear to All – accessible information guidance and support
How to Use the NHSGGC Telephone Interpreting Service to contact our services – Patient Leaflet in 40 languages
Patient Experience and Public Involvement (PEPI) – NHSGGC
Datix Incident reporting system
Interpreting & Language Resources
Meeting the needs of Autistic people and people with other types of neurodivergence
This information is for all staff involved in the treatment and care of Autistic patients and patients with other types of neurodivergence.
Using these guidelines will help ensure that neurodivergent people are enabled to access services and undergo treatments in a manner which fully addresses their needs. This information is also available on the Right Decisions app.
What is Neurodiversity?
Neurodiversity is the term that explains the natural variation in everyone’s brain, including thinking processes, information processing and learning approaches.
We’re all neurodiverse – all our brains are different. However, over 15% of people in the UK, or roughly 1 in 7 individuals, are neurodivergent.
A neurodivergent person’s brain processes information differently from what is considered typical for most people. Autism, attention deficit disorders (ADHD), dyslexia and dyspraxia are some examples of the most widely recognised neurodivergent conditions.
Most neurodivergent conditions are experienced within a spectrum – meaning that the experience will differ from person to person. A person can also identify with more than one type of neurodivergence.
Neurodivergent conditions tend to be invisible, which can create barriers for individuals in accessing the support they may need to thrive in society.
The concept of neurodiversity recognises the value of each variation making up the range of human thinking, whether it be neurotypical or neurodivergent.
It is important to use inclusive language when discussing neurodiversity, and individuals’ personal choices on how they identify should always be respected. However, identity-first language is generally preferred among neurodivergent communities, such as saying ‘autistic people’ rather than ‘people with autism’.
Autism
What is Autism?
“Autism is a lifelong developmental disability which affects how people communicate and interact with the world”.
“Autism is not a disorder… it is a neurological difference: one with a unique way of thinking and experiencing the world.”
These quotes indicate the range of opinion which exists when seeking to define Autism or being Autistic. One firmly describes Autism as a deficit based disability whilst the other considers Autism as part of the broad range of neuro types (Neurodiversity) which exist in the world.
You may often hear the term “Autism Spectrum” which reflects the range of ways someone can experience being Autistic. It is different for everyone. Some people will require very little or no support with their day to day life whilst others may live in a supported environment. Many people will have levels of support somewhere in between and these needs may vary over time.
Identifying Needs – the Autistic SPACE Framework
The variability in the experiences of Autistic people can make it difficult to create a standardised approach to patient care. The Autistic SPACE framework has been developed by Autistic Doctors International to encompass the breadth of autistic experience and healthcare access needs.
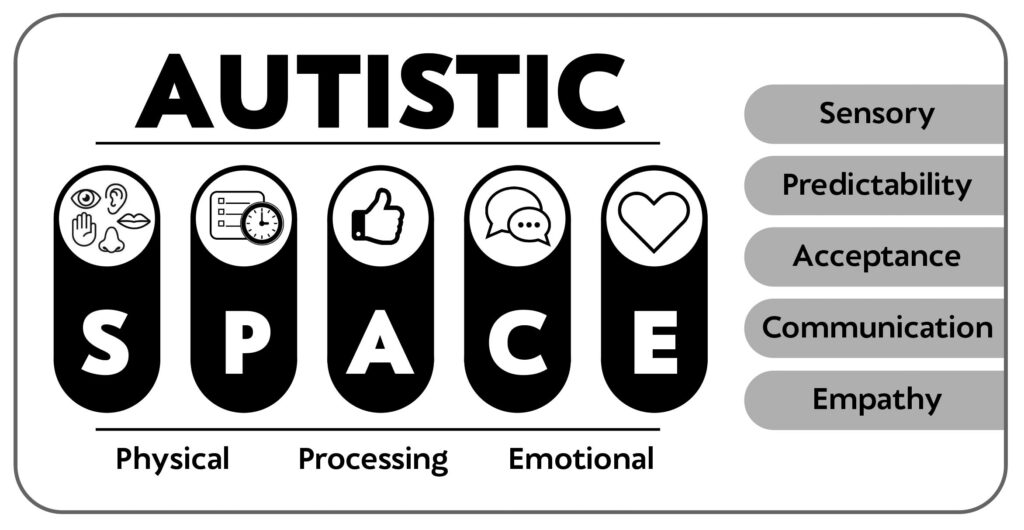
Sensory needs – Sensory sensitivities are common to almost all Autistic people but the type of and degree to which people experience these varies. Hypo or hyper-reactivity to any sensory stimuli is possible and can vary contextually.
Predictability – Access to healthcare is best maximised for Autistic people when the environment and context is made as known and predictable as possible. Sudden or unplanned change is particularly difficult.
Acceptance – It is important to have a holistic approach, in which Autistic characteristics are understood and accepted.
Communication – Autistic people communicate differently. Many use fluent speech, but may experience challenges with verbal communication at times of stress or sensory overload. Others may be non/minimally speaking and use augmentative and alternative communication methods, including visual cards, writing or electronic devices.
Empathy – Autistic people do not lack empathy but it may be experienced or expressed differently from people who are not Autistic.
Physical, Emotional and Processing Space
Autistic people may need more physical space. Proximity to others, particularly within touching distance, is often difficult to tolerate.
Identifying, processing and managing emotions can be challenging, particularly when Autistic ways of expressing emotions are not understood. Sensory overload or overwhelming emotions may lead to Autistic meltdown or shutdown. Considering this will minimise risks, but if it occurs, the best approach is often to allow space to recover.
Understanding that Autistic people may need additional time to process new information or unexpected changes when compared to non-Autistic people is invaluable in improving the accessibility of healthcare.
Autistic Meltdowns/Shutdowns
A meltdown is an intense response to an overwhelming situation. It happens when someone becomes completely overwhelmed by their situation and can lead to a temporarily loss of control of their behaviour.
Whether in terms of outward expression (meltdown) or inward expression (shutdown), this is often brought about by lack of consideration of the Autistic SPACE principles outlined here.
Neither of these things should be viewed as challenging behaviour but if they do occur the best approach is often to allow space for the person to recover.
Experiencing persistent meltdowns/shutdowns can lead to Autistic burnout, characterised by pervasive, long-term exhaustion, loss of function, and reduced tolerance to stimulus. Application of the Autistic SPACE principles can help go some way to reducing this. For further information and advice on Autistic meltdowns, see the National Autistic Society website.
Other types of neurodivergence
Attention Deficit Hyperactivity Disorder (ADHD):
Refers to a group of behavioural symptoms which include difficulty concentrating and paying attention, hyperactivity and impulsiveness
Dyslexia
Difficulties in learning to read, write and/or spell, including reading and writing. A Dyslexic person can also have associated problems such as remembering and processing information.
Dyspraxia – Also known as Developmental Coordination Disorder (DCD).
Affects physical coordination and balance.
Can also affect working memory and cause difficulties of organisation and planning
Dyscalculia
Makes it difficult to understand and work with numbers, perform calculations, and remember mathematical facts.
Addressing barriers
Research tells us that a range of barriers to accessing and receiving health services exist for neurodivergent people.
These will vary from person to person, so it is important to have open communication to ensure that you understand what the issues may be and how best to address them.
Examples could be –
Staff not understanding condition
Find out about the person’s condition and how it affects them. Gain better knowledge through training opportunities.
Not feeling listened to
Give the time necessary to listen to the person’s experience and clarify any information given.
Use advocates where necessary.
Uncertainty/anxiety
Provide clear information about what to expect. Provide the opportunity for the person to ask questions ahead of particular appointments.
Difficulties with concentration
Too much information and complex language causes issues for most patients. Ensure your information is provided in stages, is clear and simple and is being understood at each point of delivery.
Many of the adjustments that should be considered at each part of the patient’s journey will apply to patients with other types of neurodivergence. See the Autism Acute Patient Pathway for more detailed examples.
Acute Patient Pathway
Issues to consider
This pathway focuses on measures that should be considered at each part of the patient journey to address possible barriers and concerns for Autistic people.
Many of these issues will apply to patients with other types of neurodivergence. Each person’s experience will be different – it is therefore important to communicate with patients to learn their individual needs.
Pre-admission
Give as clear a picture as possible of what the person can expect to happen.
- Information (in appropriate formats) should include an explanation of processes and medical terminology. It should also, where possible, include routes to buildings/clinics from point of arrival at the hospital.
- If there is sufficient advance notice of the admission, offer the opportunity for a pre visit or additional information to reduce anxiety levels about the experience. This will also aid staff understanding of what is required to improve a patient’s journey.
- If it is an outpatient appointment, try to give an Autistic person appointments at less busy times of day. This may help reduce stress levels caused by busy environments.
Admission
- Is the reception desk in a noisy or brightly lit area? Is there a lot of information for the Autistic person to process? Consider using a quieter, less brightly lit space for admission and allow time for the person to ask questions and process what they are being told.
- If there has been no opportunity to chat or answer questions prior to admission, staff should take extra time to ensure the Autistic person (and where relevant their family/carer/partner) has understood what is happening. Speak clearly, giving the Autistic person time to process the information. If someone is non-verbal do not assume that they do not understand what is being said.
During Stay
- If the waiting area is brightly lit or noisy consider the use of a quieter, less brightly lit space. Also take into account any smells; is it possible to minimise this?
- Consider where the Autistic person will be during their stay in terms of lights, sounds and smells. If necessary try to allocate a quieter less brightly lit space away from strong smells.
- Explain any examinations or processes to be undertaken during the stay. If an Autistic Person has a carer, enlist their support but do not talk over the Autistic Person.
- Any changes which need to be made should be clearly explained to the person as soon as possible. This will give time to enable an Autistic person to process the changes and feel more comfortable.
- If it is not possible to find an alternative space, consider what can be done to lessen the environment and sensory influences. A single room can be easier in terms of lessening light, sound and smell. Encourage use of noise cancelling earphones or ear buds. – Many Autistic people will have these but may not be sure of using them in the environment; consider providing such equipment. Some Autistic people also wear dark glasses to lessen the impact of bright light.
- Ensure that the Autistic Person is aware of the position of other relevant facilities such as toilets (Accessible toilets if necessary).
- Over-stimulation of an Autistic Person’s senses may lead to “stimming”. Stimming is a self-regulatory behaviour intended to soothe or steady an Autistic Person. This can take many forms including humming, rocking and hand-wringing or flapping but will vary from Autistic person to Autistic person. It may also involve the use of stimming tools (sometimes called stim toys) such as fidget spinners or rings and squishy toys or just something the person finds comforting. Not all Autistic people visibly stim and it may go unnoticed by others if it takes a less visible form.
- Be aware that a previously vocal person can also shut down when under stress, becoming less able to communicate.
Discharge
When the appointment or hospital stay is over, be clear about what will happen next, including any timescales and the need for follow up.
Take time to go through any information that an Autistic person may need and ensure that it is in a format which is suitable for them. Go through the information with the person if necessary, ensuring you check their understanding. Take special care to ensure any medical terminology is explained.
Good Practice example – RAH Day Surgery
Autistic patients can enter the unit via an alternative entrance which enables a less stressful start to their appointment/stay.
Within their six bedded wards, staff at can pull their dark curtains around individual beds to create more privacy and lessen sensory input. They can also reduce lighting in the individual areas.
Supporting Information
Neurodiversity/Neurodivergence
NHSGGC – Supporting and Working with our Neurodivergent Colleagues
Autism
What is Neurodiversity & How Does it Relate to Autism? –
Autistic SPACE: a novel framework for meeting the needs of autistic people in healthcare settings
Understanding autistic burnout
The Patient Rights (Scotland) Act 2011
Autism/ADHD
Challenges Autistic and ADHD People Face in Healthcare and What Can Help –
ADHD
Attention deficit hyperactivity disorder: What is it?
Dyslexia, Dyscalculia, Dyspraxia
Dyslexia Scotland Dyslexia Scotland has a confidential dyslexia Helpline. Which is available Monday-Thursday 10.00-4.30, Friday 10.00-4.00 on 0344 800 8484 or helpline@dyslexiascotland.org.uk
British Dyslexia Association Also has information re Dyscalculia
