Why immunise?
The development of effective vaccines has led to a huge decrease in childhood deaths. The World Health Organization (WHO) states: ‘The 2 public health interventions that have had the greatest impact on the world’s health are clean water and vaccines.’
Benefits for you
As children develop they’re exposed to many risks, one of these risks being infections. Most of these will cause mild illnesses. However, despite great medical advances, infection can still cause severe illness, disability and, at times, death.
Before vaccines were available, many children in the UK died from diseases such as whooping cough, measles and polio. Despite successful immunisation programmes, the diseases that vaccines protect against do still exist.
The benefit of immunisation is that your child has the best possible protection against dangerous diseases. This can give you peace of mind.
Pre-School Children
The 6-in-1 Vaccine
Overview
The 6-in-1 vaccine, also commonly known as the DTaP/IPV/Hib/HepB vaccine, helps protect your child against:
What’s pertussis (whooping cough)?
Whooping cough is a disease that can cause long bouts of coughing and choking, making it hard to breathe. Whooping cough can last for up to 10 weeks.
Babies under one year old are most at risk from whooping cough. For these babies, the disease is very serious and can kill. It’s not usually as serious in older children. Before the pertussis vaccine was introduced, on average 120,000 cases of whooping cough were reported each year in the UK.
What’s diphtheria?
Diphtheria is a serious disease that usually begins with a sore throat and can quickly cause breathing problems.
It can damage the heart and nervous system and, in severe cases, can kill. Before the diphtheria vaccine was introduced in the UK, there were up to 70,000 cases of diphtheria a year, causing around 5,000 deaths.
What’s tetanus?
Tetanus is a disease affecting the nervous system that can lead to muscle spasms, cause breathing problems and even kill. It’s caused when germs that are found in soil and manure get into the body through open cuts or burns.
Tetanus can’t be passed from person to person.
What’s polio?
Polio is a virus that attacks the nervous system and can cause permanent paralysis of the muscles. If it affects the chest muscles or the brain, polio can kill.
Before the polio vaccine was introduced, there were as many as 8,000 cases in the UK during the polio epidemic. Because of the continued success of the polio vaccination, there have been no cases of paralytic polio in the UK for nearly 40 years (the last case was in 1984). Polio remains a threat with poliovirus traces found in London sewage in early 2022.
Being fully vaccinated is the best way to protect against becoming ill from polio. It’s important to make sure you and your child are up to date with your vaccines.
What’s Hib?
Hib is an infection caused by haemophilus influenzae type b bacteria. It can lead to a number of major illnesses such as blood poisoning (septicaemia), pneumonia and meningitis. The illnesses caused by Hib can kill if they’re not treated quickly. Before the Hib vaccine was introduced, there were about 800 cases of Hib in young children every year in the UK.
The Hib vaccine only protects your baby against the type of meningitis caused by the haemophilus influenzae type b bacteria – it doesn’t protect against any other type of meningitis.
More about haemophilus influenzae type b (Hib)
What’s hepatitis B?
Hepatitis B (HepB) is a virus that infects the liver. Many people with HepB infection have no symptoms and don’t know they’re infected. Others have flu-like symptoms and yellowing of the skin (jaundice).
In children, HepB can persist for years and may eventually cause serious liver damage.
Why should my baby be vaccinated?
Babies can catch these serious diseases from birth, so it’s important to protect them as soon as possible.
When will my baby be immunised?
All babies are eligible for the vaccine free on the NHS.
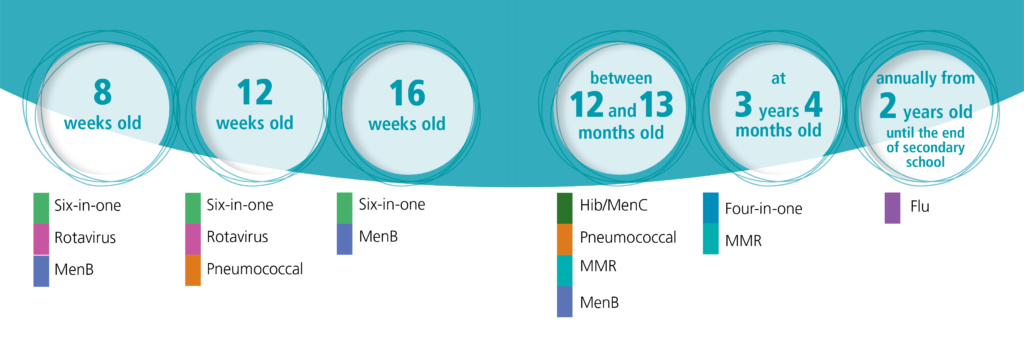
Your baby will be offered the 6-in-1 vaccine around 8, 12 and 16 weeks of age. Your local NHS immunisation team will contact you to let you know about their arrangements for your baby’s routine childhood immunisations.
Most NHS immunisation teams run special immunisation baby clinics. If you can’t get to the clinic, contact your local NHS immunisation team to make another appointment.
Meningitis B (MenB) vaccine
Overview
The meningitis B (MenB) vaccine helps protect against meningitis and septicaemia (blood poisoning) caused by meningococcal bacteria B.
What’s meningitis?
Meningitis is inflammation of the lining of the brain and spinal cord. This causes pressure on the brain resulting in symptoms like:
- severe headache
- stiff neck
- dislike of bright light
- drowsiness
- convulsions/fits
Meningitis can progress very rapidly and can lead to:
- deafness
- blindness
- epilepsy
- learning difficulties
It can even lead to death.
What’s septicaemia (blood poisoning)?
Septicaemia (blood poisoning) is a serious, life-threatening infection that gets worse very quickly. The risk of death is higher compared to meningitis.
The signs of cold hands and feet, pale skin, vomiting and being very sleepy or difficult to wake can come on quickly.
More about meningitis and septicaemia
Charlotte’s story: meningococcal septicaemia (MenB)
Charlotte developed septicaemia (serious blood poisoning) through type B meningococcal disease (MenB) in 2010, before the MenB vaccine was introduced in the UK. Her mother Jenny talks about the impact on Charlotte and the rest of her family.
How common is type B meningoccocal disease?
MenB is now the cause of most cases of meningococcal disease in Scotland. Although this infection isn’t common, MenB is extremely serious and can lead to permanent disability and death. The meningococcal bacteria can also cause local outbreaks in nurseries, schools and universities.
Why should a baby be vaccinated?
MenB infection is most common in babies and young children. This is because their immune systems aren’t yet fully developed to fight off infection. The highest number of cases are in babies around 5 months of age. This is why the first immunisations are offered to babies younger than this and have to be given at 2 and 4 months of age.
This vaccine helps protect babies against MenB, There are other vaccines, like MenC, that protect against some other types of meningococcal infections.
Who is eligible for the vaccine?
The MenB vaccine is routinely offered to all babies at 8, 16 weeks, and 12 to 13 months.
When will a baby be immunised?
The MenB vaccine has been part of the routine childhood immunisation programme in Scotland since 1 September 2015. Your local NHS immunisation team will send you an appointment to bring your child in for their routine childhood immunisations.
Babies will be offered the MenB vaccine when they come in for their other routine immunisations at 8, 16 weeks and 12 to 13 months.
Find out how to contact your local NHS immunisation team regarding your vaccination appointment
If a baby is due their MenB vaccine, please ask your pharmacist about paracetamol for them. Fever can be expected after any vaccine but is more common when the MenB vaccine is given with the other routine immunisations at 8 and 16 weeks of age. This is why it’s recommended that babies gets infant paracetamol when getting these immunisations to prevent and treat fever.
Rotavirus vaccine
Overview
The rotavirus vaccine helps protect babies against rotavirus.
What’s rotavirus?
Rotavirus is a virus that infects the gut (tummy), causing severe diarrhoea and vomiting. Most babies get sick (vomit) or have diarrhoea at some time and recover fully after a few days. However, sickness and diarrhoea caused by rotavirus can lead to dehydration (loss of body fluids). Dehydration can be very dangerous for babies and young children and can require hospital treatment.
Before the vaccine was introduced in 2013, around 1200 babies in Scotland had to go to hospital every year with rotavirus.
Why should a baby be vaccinated?
The rotavirus immunisation protects a baby against this illness.
The most important thing you can do is have the baby immunised against rotavirus, as part of the Routine Childhood Immunisation Programme in Scotland.
In countries where babies already get the rotavirus vaccine there’s been a big drop in the number of babies and young children going to hospital because of the virus.
With lots of younger babies having the immunisation the chances of it spreading are reduced. Rotavirus causes fewer problems in older children, and it’s rare in adults.
When will a baby be immunised?
The rotavirus immunisation is offered to all babies in Scotland.
The rotavirus vaccine is normally given with the baby’s other routine immunisations at 8 weeks and again at 12 weeks of age. Your local NHS immunisation team will invite you for the vaccination, so there’s no need to book an appointment.
Pneumococcal vaccine for babies
Overview
The pneumococcal vaccine helps protect against illnesses and conditions caused by pneumococcal bacteria.
What illnesses and conditions are caused by pneumococcal bacteria?
Pneumococcal infection is caused by pneumococcal bacteria. It can cause serious illness such as pneumonia, and is one of the most common causes of meningitis (an infection of the lining of the brain).
Pneumococcal infection can cause:
- bronchitis
- ear and sinus infections
- a life-threatening infection of the blood (septicaemia)
- meningitis
- pneumonia (which can also be life-threatening).
Children under 2 years of age and children with certain health conditions have a higher chance of becoming unwell with pneumococcal infection.
How common are pneumococcal bacteria?
Up to 60% of children carry pneumococcal bacteria in the back of their nose and throat. They constantly pass these bacteria around by coughing, sneezing and close contact.
Why should a baby be vaccinated?
The pneumococcal vaccine provides some protection against meningitis caused by pneumococcal infection, and against other conditions such as severe ear infections and pneumonia caused by pneumococcal bacteria.
This vaccine doesn’t protect against meningitis caused by other bacteria or viruses.
Who is eligible for the vaccine?
Some children are at an increased risk from pneumococcal infection. All at risk children will be offered the vaccine according to the routine childhood immunisation programme. If you aren’t sure about your child’s health or need further advice, speak to your health professional.
When will a baby be immunised?
If a baby is eligible, they will be offered the pneumococcal vaccine when they’re 12 weeks old, with a booster dose given between 12 and 13 months. The pneumococcal booster dose between 12 and 13 months is usually given at the same time as the Hib/MenC, MMR and MenB vaccines.
In addition to this some children and adults aged from 2 to 64 years old, who are at a higher risk of developing a pneumococcal infection than the general population, will be offered additional pneumococcal vaccinations.
Your local NHS immunisation team will contact you to let you know about their arrangements for the baby’s routine childhood immunisations.
Hib Men C
Overview
The Hib/MenC vaccine helps protect a child against 2 of the causes of meningitis and septicaemia (blood poisoning). This vaccine will help protect the child through early childhood.
What is Hib?
Hib is an infection caused by Haemophilus influenzae type b bacteria. It can lead to a number of major illnesses such as septicaemia (blood poisoning), pneumonia and meningitis.
More about Haemophilus influenzae type b
What is meningitis?
Meningitis is inflammation of the lining of the brain and spinal cord. This causes pressure on the brain resulting in symptoms like:
- severe headache
- stiff neck
- dislike of bright light
- drowsiness
- convulsions/fits
Meningitis can progress very rapidly and can lead to:
- deafness
- blindness
- epilepsy
- learning difficulties
It can even lead to death.
What is septicaemia?
Septicaemia (blood poisoning) is a serious, life-threatening infection that gets worse very quickly. The risk of death is higher than with meningitis.
The signs of cold hands and feet, pale skin, vomiting and being very sleepy or difficult to wake can come on quickly.
Why should a baby be vaccinated?
A child will be offered a dose of the combined Hib/MenC vaccine between 12 and 13 months of age to:
- boost their protection against Haemophilus influenzae type b (Hib)
- help protect against meningitis and septicaemia caused by meningococcal group C (MenC) bacteria
The Hib/MenC vaccine doesn’t protect against meningitis and septicaemia (blood poisoning) caused by:
- meningococcal group B bacteria
- other bacteria or viruses such as pneumococcal or mumps
When will a baby be immunised?
A baby will be offered the Hib/MenC vaccine at 12 to 13 months. Your local NHS immunisation team will contact you to let you know about their arrangements for the baby’s routine childhood immunisations.
Most NHS immunisation teams run special immunisation baby clinics. If you cannot attend your appointment contact your NHS immunisation team to make another.
Find out how to contact your NHS immunisation team regarding the baby’s vaccination appointment
MMR
The MMR vaccine is given in 2 doses and helps protect against measles, mumps and rubella. Find out more about the vaccine, and when and where to get it.
Why should someone have the MMR vaccination?
The MMR vaccine helps to protect people against measles, mumps and rubella. It’s sometimes also offered to adults who missed their childhood immunisations.
Measles, mumps and rubella are highly infectious diseases. They can cause serious medical complications.
A high number of people in Scotland have had the MMR vaccine. This means there’s been a big reduction in the number of people catching these diseases.
Who is eligible for the MMR vaccine?
All babies and children in Scotland are eligible for the MMR vaccine.
They’ll be offered the MMR vaccine in 2 doses:
- the first between 12 and 13 months
- the second at 3 years 4 months
Although normally given at these times, if it’s missed, it can be given at any age.
Some young people and adults who missed out on their MMR vaccine may also be eligible, like those who are a planning a pregnancy. If you didn’t have 2 doses of the MMR vaccine as a child, you can contact your local NHS immunisation team to discuss your eligibility.
The 4-in-1 Vaccine
Overview
The 4-in-1 vaccine, also known as the DTaP/IPV or dTaP/IPV vaccine, helps protect your child against:
- pertussis (whooping cough)
- diphtheria
- tetanus
- polio
What’s pertussis (whooping cough)?
Whooping cough is a disease that can cause long bouts of coughing and choking, making it hard to breathe. Whooping cough can last for up to 10 weeks.
Babies under one year are most at risk from whooping cough. For these babies, the disease is very serious and can kill. It’s not usually as serious in older children.
Whooping cough germs can be spread from person to person through close contact.
What’s diphtheria?
Diphtheria’s a serious disease that usually begins with a sore throat and can quickly cause breathing problems. It can damage the heart and nervous system and, in severe cases, can kill.
Diphtheria germs are spread from person to person through close contact.
What’s tetanus?
Tetanus is a disease affecting the nervous system that can lead to muscle spasms, cause breathing problems and even kill.
It’s caused when germs found in soil and manure get into the body through open cuts or burns. Tetanus can’t be passed from person to person.
What’s polio?
Polio is a virus that attacks the nervous system and can cause permanent paralysis of the muscles. If it affects the chest muscles or brain, polio can kill.
The polio virus is usually spread from person to person, or by swallowing contaminated food or water.
Before the polio vaccine was introduced, there were as many as 8,000 cases in the UK during the polio epidemic. Because of the continued success of the polio vaccination, there have been no cases of paralytic polio in the UK for nearly 40 years (the last case was in 1984). Polio remains a threat with poliovirus traces found in London sewage in early 2022.
Being fully vaccinated is the best way to protect against becoming ill from polio. It’s important to make sure you and your child are up to date with your vaccines.
Why should my child be vaccinated?
The vaccine boosts the immunisations that were given to your child at 8, 12 and 16 weeks of age – boosting protection against pertussis (whooping cough), diphtheria, tetanus, and polio.
Who is eligible for the vaccine?
This vaccine’s offered to children aged over 3 years 4 months at the same time as they are offered the MMR vaccine. It’s also used for a primary course of immunisation in children over 10 years old and adults.
When will my child be immunised?
Your child will be offered the 4-in-1 vaccine at around 3 years and 4 months. Your local NHS immunisation team will contact you to let you know about their arrangements for your child’s routine childhood immunisations.
Most NHS immunisation teams run special immunisation clinics. If you can’t get to the clinic, contact your local NHS immunisation team to make another appointment.
Young people in Secondary School/not in mainstream education
HPV Vaccine – S1 to S6
What the HPV vaccine is for
Immunisation (vaccination) information in other languages
Evidence shows the HPV vaccine helps protect people from HPV-related cancers. The human papillomavirus (HPV) vaccine is offered to every S1 pupil in Scotland.
Getting the vaccine now protects you against future risks. HPV can lead to cancers like:
- head and neck cancers
- cervical cancer
- anogenital cancers – for example, anal, penile (penis) cancer, cancer of the vagina, and cancer of the vulva
The HPV vaccine also protects you against over 90% of genital wart infections.
Who can get the HPV vaccine
Every person in Scotland aged 11-13 will be offered the HPV vaccine free of charge.
You should not have some vaccines if you’ve had a confirmed serious (anaphylactic) reaction to:
- a previous vaccine
- any ingredient of the vaccine
About the HPV vaccine
The GARDASIL 9 vaccine is used in Scotland.
Gardasil 9 helps protect against 9 types of HPV.
The vaccine protects against HPV types 16 and 18, which are the cause of most cervical cancers in the UK (more than 80%). The vaccine also protects against types 31, 33, 45, 52 and 58, which cause an additional 15% of cervical cancers.
The vaccine also protects against 2 other types of HPV. These cause around 90% of cases of genital warts.
The HPV vaccine is not a live vaccine. It cannot cause HPV.
The vaccine is the safest and most effective way to protect against HPV.
How to get the HPV vaccine
You’ll be offered the HPV vaccine as part of the school-based immunisation programme. Vaccines are given by your local NHS immunisation team.
Your school will tell you when vaccination sessions are taking place.
Find out more about the vaccinations you’ll be offered at school
If you have any questions on the day, you can speak to the person giving you the vaccine.
If you missed your vaccination and you’re still at school
If you miss your HPV vaccination, there will be further opportunities to get it. For example, you may be offered a rescheduled vaccination appointment next year.
If you’re unsure if you’ve missed any other vaccines, you should
first check your red book. If you do not have a red book, or it has gone missing, you can check with your local NHS immunisation team.
Young people not in mainstream education
You’re also eligible for the HPV vaccine if you’re:
- educated at home
- not in mainstream education
Please contact your local NHS immunisation team to arrange your appointment.
If your child is home schooled and has missed out on any vaccinations and you with them to be vaccinated. Then please ask your GP Practice to refer you to the Child Vaccination Team for this. On receipt of the referral the team will be in touch with you to arrange this.
If you’ve missed your vaccination and have now left school
If you’ve left school and you didn’t get your HPV vaccine when you were eligible, you may still be able to get it up until you turn 25.
This only applies to:
- people who are currently eligible
- boys who became eligible from the 2019/2020 academic year
- girls under 25 who were eligible under routine and catch up programmes introduced in 2008
Your local NHS immunisation team can confirm if you’re eligible. They can also explain how to get the HPV vaccine in your area.
If you / your child does not attend school or has missed vaccinations given in school, please contact the School Team listed under FAQs ‘School Team Contact Details’.
The vaccine consent form
You should be given a consent form and leaflet by your school. You and your parent or carer should chat about the information. Both you and your parent or carer should sign the consent form and return it to your school. You should return the consent form even if you’re not going to have the vaccine.
We recommend you get agreement from your parent or carer, but it isn’t always necessary.
MMR Vaccine – S1 – S6
The MMR vaccine is given in 2 doses and helps protect against measles, mumps and rubella. Find out more about the vaccine, and when and where to get it.
Why should someone have the MMR vaccination?
The MMR vaccine helps to protect people against measles, mumps and rubella. It’s sometimes also offered to adults who missed their childhood immunisations.
Measles, mumps and rubella are highly infectious diseases. They can cause serious medical complications.
A high number of people in Scotland have had the MMR vaccine. This means there’s been a big reduction in the number of people catching these diseases.
Who is eligible for the MMR vaccine?
All babies and children in Scotland are eligible for the MMR vaccine.
They’ll be offered the MMR vaccine in 2 doses:
- the first between 12 and 13 months
- the second at 3 years 4 months
Although normally given at these times, if it’s missed, it can be given at any age.
Some young people and adults who missed out on their MMR vaccine may also be eligible, like those who are a planning a pregnancy. If you didn’t have 2 doses of the MMR vaccine as a child, you can contact your local NHS immunisation team to discuss your eligibility.
If you / your child does not attend school or has missed vaccinations given in school, please contact the School Team listed under FAQs ‘School Team Contact Details’.
If your child is home schooled and has missed out on any vaccinations and you with them to be vaccinated. Then please ask your GP Practice to refer you to the Child Vaccination Team for this. On receipt of the referral the team will be in touch with you to arrange this.
DTP Vaccine – S3 to S6
The DTP vaccine provides protection against diphtheria, tetanus and polio. The vaccine is usually given in S3 (around 14 years old). Find out when and where to get it.
What the DTP vaccine is for
Immunisation (vaccination) information in other languages and formats
The DTP vaccine protects against diphtheria, tetanus and polio. These are serious diseases.
You need a total of 5 doses of the diphtheria, tetanus and polio vaccine to build up immunity and give you longer-term protection.
You should have had:
- the first 3 doses as a baby
- the fourth dose before you started primary school (after turning 3 years and 4 months)
You should have the fifth dose in S3 (around 14 years old).
What’s diphtheria?
Diphtheria is a serious disease that usually begins with a sore throat. It can quickly cause breathing problems. It can also damage the heart and nervous system, and in severe cases, can kill. Diphtheria is passed from person to person through close contact.
Before the diphtheria vaccine was introduced in the UK, there were up to 70,000 cases of diphtheria a year. These caused around 5,000 deaths.
What’s tetanus?
Tetanus is a painful disease affecting the nervous system that can lead to:
- muscle spasms
- breathing problems
- death
It’s caused by germs found in soil and manure getting into the body through open cuts or burns.
Tetanus can’t be passed from person to person.
What’s polio?
Polio is a virus that attacks the nervous system and can cause permanent paralysis of muscles. If it affects the chest muscles or the brain, polio can kill. The polio virus is usually spread from person to person or by swallowing contaminated food or water.
Before the polio vaccine was introduced, there were as many as 8,000 cases in the UK during the polio epidemic.
Who can get the DTP vaccine
All young people in S3 (around 14 years old) are eligible for the vaccination. This is part of their routine immunisation schedule.
- If you were immunised as a child – The DTP vaccine completes the 5 dose course against diphtheria, tetanus and polio. Although you’ve already had 4 doses of diphtheria, tetanus and polio vaccines, , you need a total of 5 to build up your immunity and provide longer-term protection.
- Reasons you should not have the vaccine – here are very few young people who can’t have the DTP vaccine. You shouldn’t have the vaccine if you’ve had a confirmed anaphylactic reaction to:
- a previous vaccine
- any ingredient of the vaccine
- neomycin, streptomycin or polymyxin B (antibiotics that may be added to vaccines in very tiny amounts)
- If you have a bleeding disorder – If you have a bleeding disorder, tell the person giving you the vaccine. They’ll give the injection in a slightly different way that will be better for you.
About the DTP vaccine
The REVAXIS vaccine is routinely used in Scotland.
The DTP vaccine is not a live vaccine. It cannot cause the diseases it protects against.
The DTP vaccine is the safest and most effective way to protect against serious diseases.
How to get the DTP vaccine
You’ll be offered the DTP vaccine when you’re in S3 (around 14 years of age) at school. Vaccines are given by your local NHS immunisation team. Your school will tell you when vaccination sessions are taking place.
Find out more about the vaccinations you’ll be offered at school
If you have any questions on the day, you can speak to the person giving you the vaccine.
If you / your child does not attend school or has missed vaccinations given in school, please contact the School Team listed under FAQs ‘School Team Contact Details’.
If your child is home schooled and has missed out on any vaccinations and you with them to be vaccinated. Then please ask your GP Practice to refer you to the Child Vaccination Team for this. On receipt of the referral the team will be in touch with you to arrange this.
Meningitis ACWY (MenACWY) vaccine – S3 to S6
The meningitis ACWY (MenACWY) vaccine helps protect against meningitis and septicaemia (blood poisoning). Find out more about the MenACWY vaccine, and when and where to get it.
What the Meningitis ACWY (MenACWY) vaccine is for
Immunisation (vaccination) information in other languages and formats
The meningitis ACWY (MenACWY) vaccine helps protect against meningitis and septicaemia (blood poisoning), which are caused by meningococcal bacteria A, C, W and Y.
Young people have a higher risk of getting meningococcal disease. You’ll be offered immunisation to protect yourself and others around you.
Meningitis and septicaemia are very serious diseases. They can cause permanent disability and death. The symptoms can come on quickly.
Who can get the MenACWY vaccine
The MenACWY vaccine is routinely offered to all young people in S3 (around 14 years of age). If you’re over 14 and not already immunised, you may also be offered the vaccine.
You should not have some vaccines if you’ve had a confirmed anaphylactic shock (serious allergic reaction) to:
- a previous vaccine
- any ingredient of this vaccine
About the MenACWY vaccine
The following vaccines are routinely used in Scotland:
- Menveo Meningococcal Group A, C, W135 and Y conjugate vaccine
- Nimenrix powder and solvent for solution for injection in pre-filled syringe
The MenACWY vaccine is highly effective at protecting against the serious infections caused by meningococcal bacteria A, C, W and Y.
The MenACWY vaccine is not a live vaccine. It cannot cause meningitis.
The MenACWY vaccine is the safest and most effective way to protect against meningococcal A, C, W and Y.
How to get the MenACWY vaccine
Vaccines are given by your local NHS immunisation team. Your school will tell you when vaccination sessions are taking place.
Find out more about the vaccinations you’ll be offered at school
If you have any questions on the day, you can speak to the person giving you the vaccine.
If you missed your vaccination at school
If you missed your MenACWY vaccination, there will be further opportunities to get it. For example, you may be offered a rescheduled vaccination appointment next year.
If you’re unsure if you’ve missed any other vaccines, you should first check your red book. If you do not have a red book, or it has gone missing, you can check with your local NHS immunisation team
Young people not in mainstream education
You’re also eligible for the MenACWY vaccine if you’re:
- educated at home
- not in mainstream education
If you / your child does not attend school or has missed vaccinations given in school, please contact the School Team listed under FAQs ‘School Team Contact Details’.
If your child is home schooled and has missed out on any vaccinations and you with them to be vaccinated. Then please ask your GP Practice to refer you to the Child Vaccination Team for this. On receipt of the referral the team will be in touch with you to arrange this.
Students
You may be eligible for the MenACWY vaccination if you:
- are Scottish and attending further education in Scotland
- are aged up to 25 years old
- have not had the MenACWY vaccination
You should contact your local NHS immunisation team. They’ll advise you if it’s clinically appropriate for you to have the vaccine.
You may not be eligible for the MenACWY vaccination if you’re from outside Scotland (including other parts of the UK). You should arrange to get your vaccine before travelling to Scotland. There’s no guarantee the vaccine will be available to you after arriving in Scotland.
Seasonal Vaccination
Pre-School 6 Months to 2 Years at Risk – Flu
NHS Scotland recommends eligible children should get the flu vaccine to help protect them from influenza (flu).
Flu (influenza) is a common infectious respiratory virus. Symptoms may include a fever, a cough, a headache, and tiredness.
Why should I have my child vaccinated?
Flu can be serious. Even healthy children can become seriously ill from flu. In some cases flu can lead to complications. These can include bronchitis, pneumonia, painful middle-ear infection, vomiting, diarrhoea. In the worst cases, flu can lead to disability and even death.
Flu can be even more serious for people with health conditions such as:
- asthma
- heart, kidney, liver or neurological disease
- diabetes
- a weakened immune system
- a spleen that does not work fully
Flu can make health conditions worse.
The flu vaccine will reduce the risk of your child getting or spreading flu to friends and family who are at greater risk from flu. For example, grandparents or people with health conditions. It’ll also help prevent your child getting sick with flu and needing time off school or nursery.
How is the vaccine given?
Children aged 6 months to 2 years will be given the injectable flu vaccine.
Vaccine safety
All medicines, including vaccines, are tested for safety and effectiveness before they’re allowed to be used.
Once they’re in use, the safety of vaccines continues to be monitored by the Medicines and Healthcare products Regulatory Agency (MHRA).
The nasal spray flu vaccine has been used since 2014 and has a good safety record. Millions of doses of the vaccine have been given to children in the UK.
Does the vaccine work?
The annual vaccine offers protection against the most common types of flu virus that are around each winter. The flu vaccine should start to protect most children about 10 to 14 days after they receive their vaccination.
In previous years, the flu vaccine has worked very well, providing protection against flu. It has also reduced the chance of spreading flu into the wider community.
Pre-School 6 Months to 4 Years at Risk – Covid
NHS Scotland is offering the coronavirus (COVID-19) vaccine to children aged 6 months to 11 years at higher risk of coronavirus this spring.
To be invited for vaccination this spring, your child must have a weakened immune system and be aged 6 months to 11 years on 31 March 2024 (born on or after 1 April 2012 and before 1 October 2023).
Why is my child being offered the coronavirus vaccine?
Getting the vaccine will help to protect your child against coronavirus. The vaccine helps to build up immunity to coronavirus, so the body can fight it off more easily. If your child is vaccinated, they are much less likely to get seriously ill from coronavirus or need to go to hospital.
Infants and young children with underlying health conditions are 7 times more likely to be admitted to paediatric intensive care units with severe coronavirus, compared to those without underlying health conditions.
My child has already had the coronavirus vaccine – do they need another one?
NHS Scotland is offering a coronavirus vaccine to children at higher risk to help protect them this spring. It’s important to keep up to date with the coronavirus vaccines your child is offered.
NHS Scotland recommends coming forward every time your child is invited to keep their protection topped up.
Is the coronavirus vaccine safe?
NHS Scotland will only use a vaccine if it meets the required standards of safety and effectiveness. All medicines, including vaccines, are tested for safety and effectiveness before they’re allowed to be used. The Medicines and Healthcare products Regulatory Agency (MHRA) assesses all the data and also ensures a vaccine works and that all the necessary trials and checks have been completed.
Are there any reasons my child should not get the coronavirus vaccine?
There are very few people who cannot have the vaccine. If your child has had a confirmed severe allergic reaction (anaphylaxis) to any of the vaccine ingredients or a previous dose of the same vaccine, you should seek advice from your health professional before your child has the vaccine.
The vaccine is not a live vaccine and does not contain any animal products or egg.
Vaccine manufacturer patient information leaflets
More information about the vaccines offered, including vaccine ingredients, is available in the manufacturer patient information leaflets.
Read the coronavirus vaccine patient information leaflet for 6 months to 4 years:
Pre-School 2 – 5 year old childhood flu
NHS Scotland recommends eligible children should get the flu vaccine to help protect them from influenza (flu).
The flu vaccine is available between September and March.
Flu (influenza) is a common infectious respiratory virus. Symptoms may include a fever, a cough, a headache, and tiredness.
The flu vaccine is offered as a painless nasal spray to almost all children. It cannot give the child flu but starts to provide protection against flu within 10-14 days. The nasal spray offers the best possible protection for children and young people and can also stop flu spreading to family, friends and others, especially those most at risk of becoming seriously ill with flu. Children aged 2 to 5 are being offered vaccination from the start of the programme to ensure they receive the earliest protection and prevent the virus spreading.
Why should I have my child vaccinated?
Flu can be serious. Even healthy children can become seriously ill from flu. In some cases flu can lead to complications. These can include bronchitis, pneumonia, painful middle-ear infection, vomiting, diarrhoea. In the worst cases, flu can lead to disability and even death.
Flu can be even more serious for people with health conditions such as:
- asthma
- heart, kidney, liver or neurological disease
- diabetes
- a weakened immune system
- a spleen that does not work fully
Flu can make health conditions worse.
The flu vaccine will reduce the risk of your child getting or spreading flu to friends and family who are at greater risk from flu. For example, grandparents or people with health conditions. It’ll also help prevent your child getting sick with flu and needing time off school or nursery.
How is the vaccine given?
In Scotland, children aged 2 to 17 will usually be given the nasal spray flu vaccine. It’s quick and painless and there’s no need to sniff or inhale the vaccine. It’ll just feel like a tickle in their nose.
Children aged 2 to 17 years who cannot receive the nasal spray vaccine will receive the injectable flu vaccine.
Vaccine safety
All medicines, including vaccines, are tested for safety and effectiveness before they’re allowed to be used.
Once they’re in use, the safety of vaccines continues to be monitored by the Medicines and Healthcare products Regulatory Agency (MHRA).
The nasal spray flu vaccine has been used since 2014 and has a good safety record. Millions of doses of the vaccine have been given to children in the UK.
Does the vaccine work?
The annual vaccine offers protection against the most common types of flu virus that are around each winter. The flu vaccine should start to protect most children about 10 to 14 days after they receive their vaccination.
In previous years, the flu vaccine has worked very well, providing protection against flu. It has also reduced the chance of spreading flu into the wider community.
Primary School Children – Flu
NHS Scotland recommends eligible children should get the flu vaccine to help protect them from influenza (flu).
The flu vaccine is available between September and March.
Flu (influenza) is a common infectious respiratory virus. Symptoms may include a fever, a cough, a headache, and tiredness.
The flu vaccine is offered as a painless nasal spray to almost all children. It cannot give the child flu but starts to provide protection against flu within 10-14 days. The nasal spray offers the best possible protection for children and young people and can also stop flu spreading to family, friends and others, especially those most at risk of becoming seriously ill with flu.
Consent forms and further information will be sent home to parents and carers of school children on return to school. Secondary pupils can self-consent but are encouraged to speak to a parent or carer first. All primary and secondary school pupils with consent to be given the flu vaccine nasal spray will receive this at school starting in early September through to December 2024.
Why should I have my child vaccinated?
Flu can be serious. Even healthy children can become seriously ill from flu. In some cases flu can lead to complications. These can include bronchitis, pneumonia, painful middle-ear infection, vomiting, diarrhoea. In the worst cases, flu can lead to disability and even death.
Flu can be even more serious for people with health conditions such as:
- asthma
- heart, kidney, liver or neurological disease
- diabetes
- a weakened immune system
- a spleen that does not work fully
Flu can make health conditions worse.
The flu vaccine will reduce the risk of your child getting or spreading flu to friends and family who are at greater risk from flu. For example, grandparents or people with health conditions. It’ll also help prevent your child getting sick with flu and needing time off school or nursery.
How is the vaccine given?
In Scotland, children aged 2 to 17 will usually be given the nasal spray flu vaccine. It’s quick and painless and there’s no need to sniff or inhale the vaccine. It’ll just feel like a tickle in their nose.
Children aged 2 to 17 years who cannot receive the nasal spray vaccine will receive the injectable flu vaccine.
Children aged 6 months to 2 years will be given the injectable flu vaccine.
Vaccine safety
All medicines, including vaccines, are tested for safety and effectiveness before they’re allowed to be used.
Once they’re in use, the safety of vaccines continues to be monitored by the Medicines and Healthcare products Regulatory Agency (MHRA).
The nasal spray flu vaccine has been used since 2014 and has a good safety record. Millions of doses of the vaccine have been given to children in the UK.
Does the vaccine work?
The annual vaccine offers protection against the most common types of flu virus that are around each winter. The flu vaccine should start to protect most children about 10 to 14 days after they receive their vaccination.
In previous years, the flu vaccine has worked very well, providing protection against flu. It has also reduced the chance of spreading flu into the wider community.
Where clinics take place
Vaccinations are typically given in schools during term time. NHS GGC work with schools to communicate programme dates.
Before clinics take place, consent forms and vaccination information will be handed out to pupils at school for review at home then return to school.
If you / your child does not attend school or has missed vaccinations given in school, please contact the School Team listed under FAQs ‘School Team Contact Details’.
On the day
Pupils will usually attend clinics in the school hall or social space, class by class throughout the day.
Secondary School Children and Young People – Flu
About the programme
Immunisation is the safest and most effective way of protecting young people against serious diseases.
School-aged children are routinely vaccinated against:
- Influenza – usually offered to all primary and secondary school pupils from September to December .
The flu vaccine is offered as a painless nasal spray to almost all children. It cannot give the child flu but starts to provide protection against flu within 10-14 days. The nasal spray offers the best possible protection for children and young people and can also stop flu spreading to family, friends and others, especially those most at risk of becoming seriously ill with flu.
Consent forms and further information will be sent home to parents and carers of school children on return to school. Secondary pupils can self-consent but are encouraged to speak to a parent or carer first. All primary and secondary school pupils with consent to be given the flu vaccine nasal spray will receive this at school starting in early September through to December 2024.
https://www.nhsinform.scot/vaccineconsentyoungpeople
For details of the schedule of vaccinations in Scotland by age, please refer to NHS Inform.
Where clinics take place
Vaccinations are typically given in schools during term time. NHS GGC work with schools to communicate programme dates.
Before clinics take place, consent forms and vaccination information will be handed out to pupils at school for review at home then return to school.
If you / your child does not attend school or has missed vaccinations given in school, please contact the School Team listed under FAQs ‘School Team Contact Details’.
On the day
Pupils will usually attend clinics in the school hall or social space, class by class throughout the day.
FAQs
I am unsure of my child’s immunisation history
Please contact your GP
Pre-School Team Contact Details
Please see team contact details below:
Glasgow South/East Renfrewshire
Phone Number: 0141 577 7774 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
Health Centres: Castlemilk, Eastwood, Govanhill, Gorbals, Govanhill (EU), Pollock, Shields Centre, Elderpark, Thornliebank, Barrhead
North East/East Dunbartonshire
Phone Number: 0141 531 6635 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
Health Centres: Springburn, Kirkintilloch, Stobhill, Milngavie, Baillieston, Shettleston, Bridgeton, Townhead, Easterhouse
North West/West Dunbartonshire
Phone Number: 0141 211 6142 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
Health Centres: Dumbarton, Vale of Leven, Maryhill, Woodside, Possilpark, Community Centre for Health (CCFH), Plean Street, Drumchapel, Clydebank
Renfrewshire/Inverclyde
Phone Number: 0141 201 1056 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
Health Centres: Greenock, Port Glasgow, Johnstone, Linwood, Renfrew, Foxbar Clinic, Northcroft, Tannahill Centre, Erskine
School Team Contact Details
Please see team contact details below:
Glasgow South/East Renfrewshire
Phone Number: 0141 577 7767 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
North East/East Dunbartonshire
Phone Number: 0141 232 9838 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
North West/West Dunbartonshire
Phone Number: 0141 232 9202 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
Renfrewshire/Inverclyde
Phone Number: 0141 314 0513 (voicemail service is available)
Opening Times: Monday -Thursday 08.30am – 16.30pm and Friday – 08.30am – 16.00pm
